For the past three years, Aviva B. Sopher, MD, MS, a pediatric endocrinologist at NewYork-Presbyterian/Columbia and NewYork-Presbyterian Morgan Stanley Children’s Hospital, has been caring for a patient who, at age 11, developed anxiety and also some restricted eating. The preteen’s symptoms led him and his family on a protracted medical journey that focused on their child’s combined psychiatric diagnoses of avoidant restrictive food intake disorder and generalized anxiety disorder.
“He was initially managed with outpatient psychotherapy, but at age 14 he was started on treatment with sertraline for worsening anxiety,” notes Dr. Sopher. “His psychiatrist subsequently prescribed mirtazapine, also for anxiety, but which has the added property of increasing appetite, with the hope that he would gain weight. Unfortunately, he did not improve with these medications, and actually worsened, losing about 10 pounds.”
With his health deteriorating – including worsening symptoms of anorexia, nausea, vomiting, and anxiety – he was admitted to NewYork-Presbyterian, then transferred to the eating disorder unit of a behavioral health facility. After five days, he was transferred back to the Emergency Department at NewYork-Presbyterian Morgan Stanley Children’s Hospital for management of recurrent dehydration in the second of three back-to-back hospitalizations. He spent a week on the hospital’s pediatric hospitalist medicine service with child psychiatry consultation and discharged following adjustment of his medications and stabilization of his symptoms. Two days later, he was readmitted to NewYork-Presbyterian Morgan Stanley Children’s Hospital due to the return of his vomiting and a presyncope episode. Extensive testing revealed hyponatremia, dehydration, salt wasting, and orthostatic hypotension, and the hospital’s pediatric endocrinology service was consulted for an evaluation of his hyponatremia. Dr. Sopher was the attending on call.
Primary Adrenal Insufficiency: Unmasking a Rare but Treatable Diagnosis
“When I walked into the patient’s room, the first thing I noticed was that he had faint bronzing of his skin and he appeared very weak,” says Dr. Sopher. “The typical description of a patient with Addison’s disease is that they may look deceptively healthy because they appear to have a tan. Based on his history of low sodium levels and salt wasting and then observing the bronzed skin, number one in my differential was Addison’s (primary adrenal insufficiency). His morning cortisol level morning was 2.4 ug/dL, which is extremely low. We expect morning cortisol levels to be at least 10 ug/dL. An ACTH stimulation test performed indicated primary adrenal insufficiency as his cortisol level did not rise at all. Additionally, his ACTH level was extremely high, confirming the failing adrenal gland. The bronzed skin in primary adrenal insufficiency occurs because ACTH is metabolized melanocyte stimulating hormone”
Primary adrenal insufficiency (PAI), which is characterized by inadequate production of cortisol and aldosterone from the adrenal glands, is extremely rare in both children and adults, with a prevalence of 100 to 140 cases per million people. Symptoms of PAI are often nonspecific, analogous to what Dr. Sopher saw in her patient, and makes it challenging to uncover.
“While I knew he had some form of adrenal failure, I didn't know the exact cause,” adds Dr. Sopher. “There are several conditions that can trigger low sodium levels and/or dehydration. Classical congenital adrenal hyperplasia is the most common cause of primary adrenal insufficiency in children but is generally detected in infancy. In adolescent males, the most common etiologies, although rare, include autoimmune destruction of the adrenal gland and X-linked adrenoleukodystrophy.” With these possibilities in mind, Dr. Sopher believed that PAI was the prevailing cause and ordered tests for 21-hydroxylase antibodies and very long chain fatty acids, which test for autoimmune adrenal insufficiency and adrenoleukodystrophy respectively.
Though pediatric PAI is rare, this patient’s symptoms of fatigue, anorexia, and nausea progressing to vomiting, dehydration, hyponatremia, and hyperkalemia are a typical presentation of this disease.
— Dr. Aviva Sopher and Co-Authors, Primary Adrenal Insufficiency Masked by an Eating Disorder Diagnosis in an Adolescent Male, "JCEM Case Reports"
A Dramatic Turnaround with Treatment
“After obtaining our initial lab results, we immediately gave him stress-dose glucocorticoid with hydrocortisone, along with a considerable amount of fluids so that his salt and sugar levels could return to normal,” continues Dr. Sopher. “The most important approach with these patients is administering the glucocorticoid treatment because their body absolutely can't produce cortisol, which is essential for electrolyte balance and for normal blood pressure.”
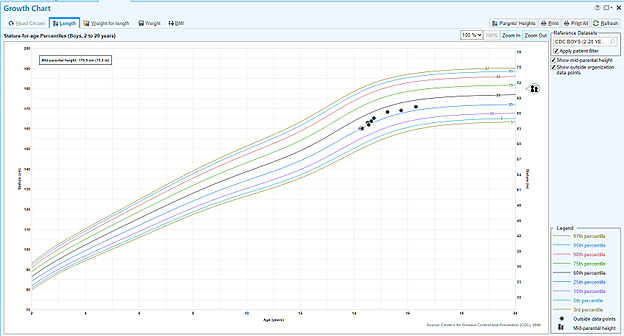
Stature-for-age percentile curve
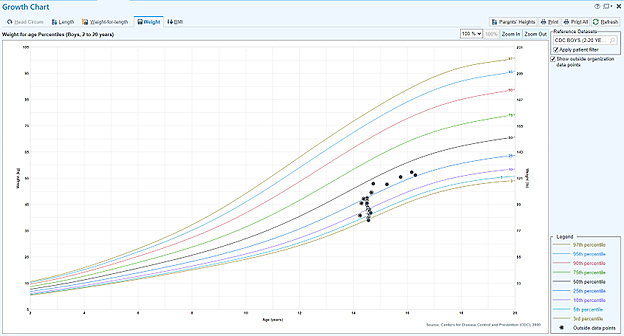
Weight-for-age percentile curve
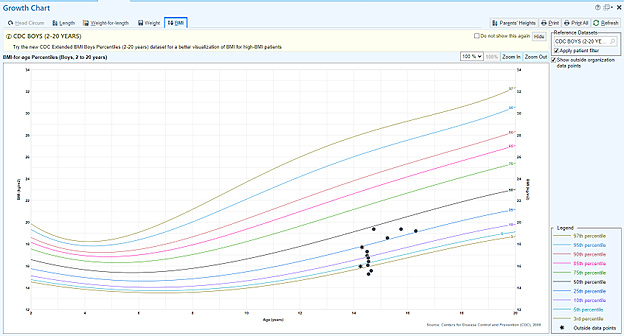
BMI-for age percentile curve
A few days after starting the hydrocortisone therapy, the patient’s nausea, anxiety, and appetite improved as did his vital signs and laboratory results. “The parents were thrilled,” notes Dr. Sopher. “Their child went from night to day. The treatment of this disease is extremely rewarding because you see a difference very quickly. Within 24 hours, his skin color went from a pale bronze to pink and he stopped vomiting. He felt better and was able to eat. When we saw him on February 4, he weighed 86 pounds. He was a skeleton. By March 12, he was 109 pounds. So, he had gained 23 pounds in just a month after being treated.”
The teenager Dr. Sopher met three years ago is now a young man of 17 leading a healthy and active life. At his last appointment a few months ago, his weight was 123 pounds, which is at the 26th percentile, and his height was five foot seven inches, the 33rd percentile. “Now his height and weight match each other, whereas before his weight was exceedingly low,” says Dr. Sopher. “In addition to the adrenal insufficiency, he was also diagnosed with hypothyroidism. It is not unusual for several autoimmune disorders to occur in the same individual. He is on a daily thyroid, mineralocorticoid and glucocorticoid replacement. He takes salt supplements intermittently as needed. He has a glucocorticoid stress dose plan for when he is ill and he wears a MedicAlert tag in the event of an emergency. He is doing very well in school and attends sailing camp in the summer. Last year, he was a counselor.”
While PAI is a lifelong condition, Dr. Sopher emphasizes that as long as patients continues following their medication regimen and are monitored by their physician, they can live totally normal and healthy lives.
A Complex Case with an Important Takeaway Message
“One of the reasons we published this article was for awareness for non-endocrinologists who would not necessarily have an endocrine cause top of mind when caring for a young patient with anxiety and manifestations of an eating disorder,” says Dr. Sopher. “We always say that patients don't walk out of textbooks, which offer perfect descriptions of disorders. It is important to remember that not every patient is a textbook case, and there may be nuances that lead you in a different direction. I am very fortunate because I work at NewYork-Presbyterian/Columbia, where there are so many people we can call on when a case isn’t making perfect sense or when a patient’s ongoing symptoms do not support the original diagnosis or responding as expected to the related treatment.”
Dr. Sopher and her co-authors conclude, “This case serves as a reminder that adrenal insufficiency must be considered in the differential diagnosis of eating disorders because signs and symptoms of adrenal insufficiency can overlap and progress insidiously. Additionally, we recognize that the diagnostic process is intertwined with a patient’s medical history and use this opportunity to discuss cognitive, specifically anchoring, bias in academic medicine.”




