Hypospadias is one of the most common congenital defects affecting the external male genitalia, with an incidence rate of about 1 in 350 males born in the United States.
The condition is defined as an insufficient development of the urethral fold and the ventral foreskin, with or without penile curvature, with the urethral opening located more proximally anywhere between the tip of the penis and the perineum.

Dr. Dix Poppas
“The urethral opening opens up prematurely underneath or on the bottom side of the phallus,” explains Dix P. Poppas, MD, Chief of Pediatric Urology at NewYork-Presbyterian Komansky Children’s Hospital and a renowned specialist in genital reconstruction. “That opening can be mild where it opens onto the glans or the coronal sulcus. It can be moderate where it opens up onto the mid-section of the shaft. Or it can be proximal where it opens between the penoscrotal junction or, the most severe, in the perineum. By far the most common form of hypospadias is the mild or the distal form. At least 50 percent of patients will have a milder form of hypospadias.”
According to Dr. Poppas, if the hypospadias is not corrected early in life, these children may have a challenge controlling their urine stream because it points down instead of straight. The diameter of the opening can often be stenotic, restricting the flow of urine. “And in the more severe forms, it can impact fertility because the sperm cannot be deposited far enough into the vagina,” says Dr. Poppas.
“As a Weill Cornell Medicine pediatric urologist, we first take a detailed exam to make sure that this is an isolated event and not associated with other potential congenital anomalies,” says Dr. Poppas. “We discuss the findings with the parents and determine whether to leave the hypospadias alone and let the child decide whether or not he wants it corrected when he is older, or the parents will decide to have the condition corrected before the child is toilet trained and aware of this issue. The ideal window for correction is between six and eight months of age in a full-term boy.”
Dr. Poppas notes that there have been well over a hundred published techniques for correcting various forms of hypospadias. “What that tells us is that no one technique has been really successful or optimal,” he says. “The choice of how you approach correcting hypospadias of a given degree is dictated by the surgeon’s experience and training and the procedure which that pediatric urologist feels most comfortable with in terms of highest success rate. Typically, the defect is corrected by building a new urethra from where the hypospadiac opening is to the tip of the penis, placing the opening in a more typical orthotopic position. In the milder forms, we use the local tissue to extend that tube. In the more severe forms or in children who have had multiple complications, we will often use either the skin from the shaft of the penis or more commonly a buccal mucosal graft.”
Building a new urethra, explains Dr. Poppas, raises the complication rates to include a fistula, one of the most common problems following hypospadias repair. “Another condition associated with hypospadias is chordee,” he says. “The more severe the hypospadias, typically the greater the degree of chordee. So, one of the most important parts of the operation is to straighten the penis so that it optimizes the length of the shaft. Once that is completed, then you build the urethra out to the tip of the penis.”
Urethral Mobilization: A Brand New, Very Old Idea
With fistulas among the most common complications following typical hypospadias repair, Dr. Poppas began to look at alternative surgical techniques that could eliminate that issue. “In the mid to late 1800s, an operation was developed called a urethral mobilization. This has subsequently been published by other pediatric urologists in the more modern era, but it just hasn’t caught on and I’m not sure why,” he says. “Over the last 12 years, I’ve been using this technique to correct mild forms of hypospadias and complications from prior hypospadias repair such as urethral fistulas. In this operation, the urethra itself is mobilized off the erectile body. You can mobilize it back to the penoscrotal junction if needed. Then, the urethra becomes pliable when it’s released, and you can stretch the urethra and secure it to the tip of the penis and then reinforce it with a vascular flap. This has eliminated urethral fistulae in my practice.”
“I have over 85 cases now with 8- to 10-year follow-up that have no fistula formation,” adds Dr. Poppas. “We are in the process of doing an IRB study looking at the outcomes compared to other forms of hypospadias repair, and we hope to have that completed by next year.”
Addressing Meatal Stenosis with the Tear Drop Approach
When Dr. Poppas first began performing urethral mobilization for hypospadias repair, he observed that the meatal stenosis rate was about 7 percent. “The meatus would scar and narrow and the children would require a second operation to correct the stenosis, which is a very simple operation, but it is still a complication,” he says. “As I thought about why that was happening, I realized that we weren’t taking a wide enough cuff of healthy tissue when we mobilized the tip of the hypospadiac meatus. I changed the technique and now when I initially mobilize the opening of the hypospadiacs urethra, I take a two- to three-millimeter cuff of epithelial tissue so that I have a much larger opening with healthy tissue to secure it to the tip of the penis. Today, our meatal stenosis rates are below 3 percent.”
Tear Drop Urethral Mobilization and Advancement Repair
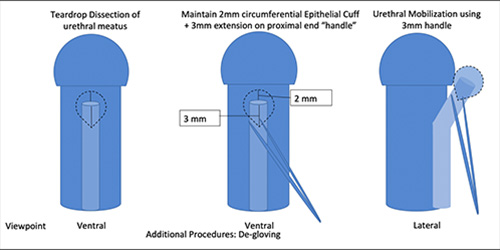
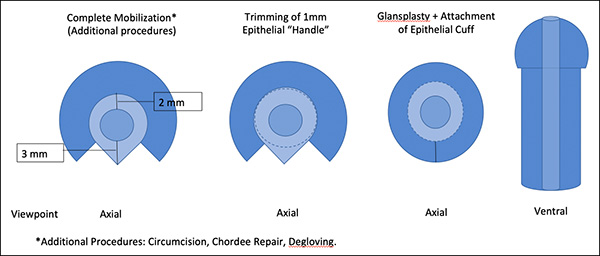
Dr. Poppas explains that the Tear Drop Urethral Mobilization and Advancement procedure, so named because of the tear drop shape of the incision, is best considered in the distal shaft to glandular level hypospadias and in re-operations where the fistula is located distally. “This modification benefits any application of the original technique because it lowers the stenosis rate,” he says. “I think it is also one of the reasons why the original operation fell out of favor, because the meatal stenosis rate was high. However, I believe this procedure will become the surgical technique of choice. The cosmetic outcomes are fantastic because you’re not using the local tissue to build the new urethra. There is a lot more tissue to work with so that the ultimate skin coverage and glans repair are much better and under less tension.”
Urethral mobilization is easy once learned and very straightforward. It offers multiple applications in both initial and in re-do repairs. The success rates are better than any other technique that I’ve used, and the cosmetic outcome is superior.
— Dr. Dix Poppas
Dr. Poppas describes another advantage of this technique. “Whenever we perform a hypospadias repair, we leave in a urethral stent so that the urine is bypassed from the reconstruction site,” he says. “In most hypospadias repairs that stent is left in place anywhere between eight and 12 days. Using this technique, I remove the stent after five days. There is less morbidity because the stent is removed sooner.”
“Urethral mobilization is easy once learned and very straightforward,” adds Dr. Poppas. “It offers multiple applications in both initial and in re-do repairs. The success rates are better than any other technique that I’ve used, and the cosmetic outcome is superior. The technique eliminates urethral fistula formation. I’ve had no urethral diverticulum, no recurrent or persistent chordee, and no wound dehiscence. The only complication I’ve had from this operation is meatal stenosis. Our goal as a surgeon is to provide the best surgical technique with the best outcome, lowest complication rates, and faster return to normal function – and urethral mobilization helps us to achieve this in mild hypospadias.”