Proximal junctional kyphosis (PJK) is a common postoperative complication following spinal deformity surgery resulting in an abnormal angulation of the vertebral column with pain and reduced function. PJK is the subject of numerous studies that often focus on several specific metrics but fail to provide comprehensive and cross-comparable results.

Dr. Joseph Lombardi
“Despite many studies investigating the causes of PJK, there still exists a poor understanding of what truly contributes to its development. More importantly, how can we identify or predict which patients are at risk for this phenomenon,” says Joseph M. Lombardi, MD, an orthopedic spine surgeon with Och Spine at NewYork-Presbyterian/
“We have a continually aging population, not only in the United States but worldwide. These patients have a higher expectation for quality of life and activity levels – even in their later decades,” says Dr. Lombardi. “As a result, we are doing more and more surgery, particularly spine and spinal fusion surgery, on elderly patients. Oftentimes these are bigger surgeries, including some that address degenerative scoliosis. While we have very good outcomes in scoliosis surgery, one particular complication that is still puzzling to the orthopedic and neurosurgery spinal community is this concept of proximal junctional kyphosis.”
According to Dr. Lombardi, radiographic criteria for PJK can be seen in 17 to 46 percent of patients following major scoliosis surgery, but not all patients do poorly or necessarily require revision surgery. “When they become symptomatic and start to have worse patient-reported outcomes, we then need to intervene,” he says.
Pinpointing the Multitude of Variables in PJK
Part of the challenge, explains Dr. Lombardi, is the number of considerations that influence development of proximal junctional kyphosis, including patient factors, such as age, baseline spinal alignment, quality of bones, tissue or muscles, and nutritional status. Other factors relate to the surgeon, including correction techniques, degree of correction, and instrumentation used. “There are so many potential variables for what can contribute to proximal junctional kyphosis that go beyond the traditional statistics that have helped us to understand it up until now,” he says.
To that end, Dr. Lombardi and his co-investigator Lawrence Lenke, MD, Surgeon-in-Chief and Co-Director of Och Spine at NewYork-Presbyterian, collaborated with a team in the Department of Computer Science at Columbia led by co-investigator Ansaf Salleb-Aouissi, PhD, to build a machine learning algorithm to identify novel metrics associated with PJK in addition to recording their strength relative to established risk factors.
“Previous studies have tried to elucidate risk factors for PJK often looking at 10 to 20 variables,” says Dr. Lombardi. “We set out to build an AI algorithm to not only answer whether traditionally identified variables are risk factors, but also to try and identify variables that previously have been unrecognized. Who are these patients at risk and how can we help prevent PJK?”
As one of the major scoliosis and spine deformity surgery centers in the United States, Och Spine at NewYork-Presbyterian has compiled a well curated internal database of patients. In their investigation, the Columbia researchers looked at 366 consecutive patients who underwent posterior spinal fusion of ≥5 vertebral levels between 2015 and 2020 with at least two years follow-up.
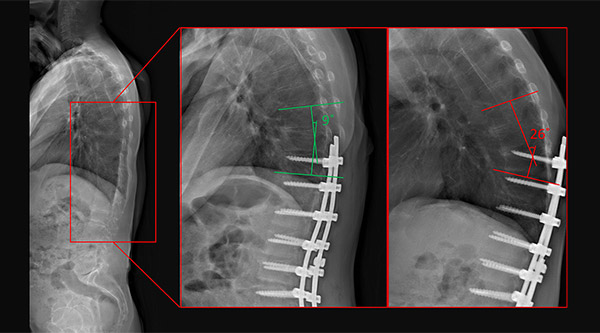
Radiology images of a patient with PJK. (Left) baseline (no hardware), (middle) immediate postoperative image (no PJK), and (right) 2.5 years follow-up image (PJK)
“We entered more than 130 different variables to build our algorithm, everything from patient characteristics to novel radiographic parameters and surgical characteristics,” says Dr. Lombardi. “In terms of our model performance, we used various algorithms, including more classic random forest and support vector models and more complex decision trees, such as XGBoosts. Ultimately, we were able to predict those patients who would develop proximal junctional kyphosis and more importantly, those who would require revision surgery.”
The Columbia study analyzed one of the largest databases to date, ultimately including 51 radiographic measurements, 10 demographic variables, and 13 surgical parameters for each of the 366 patients during the preoperative, immediate postoperative, and latest follow-up timepoints. “Our results are among the most comprehensive examination of PJK with respect to surgically relevant parameters,” says Dr. Lombardi.
Two novel parameters noted include the degree of paraspinal fatty atrophy and the posterior cranial vertical line, a plumb line drawn from the most posterior aspect of the cranium. “This is basically a vertical line that you drop from the back of the skull, and we measure that comparative to the screw at the upper-instrumented vertebrae,” says Dr. Lombardi. “We also compared it to the acetabulum as well as the ankles. We found that the posterior cranial vertical line carried a very high feature importance in predicting proximal junctional kyphosis. When we pick these points, we want it to be easily reproducible for any spine surgeon either in the operating room or in the clinic.”
Out of the 366 patients reviewed:
- 70 (19 percent) met radiographic criteria for PJK
- 21 (5.7 percent) ultimately underwent revision surgery due to proximal junctional failure
- 81 reported symptoms associated with their upper-instrumented vertebrae
“It’s one thing to be able to look back retrospectively and understand what factors cause proximal junctional kyphosis, but it is completely different to be able to develop a predictive model for who is potentially at risk in the future,” says Dr. Lombardi. “What we’re really working towards is developing an interactive, predictive model where we can sit with the patient in the office and plug in their characteristics, both from a demographic and radiographic standpoint. Our goal is to make it interactive in the sense that in real time, if we can change some of those characteristics, such as BMI or bone mineral density, we can use the algorithm to show changes to the patient’s risk for developing proximal junctional kyphosis.”
Next Steps: Designing an APP for Real-Time Risk Reduction
Dr. Lombardi and his Columbia collaborators hope to develop an app that can educate patients as to their risk and show how changes preoperatively, for example, their bone mineral density, weight, and nutrition status, can help influence or help prevent PJK. Additionally, this can be a powerful tool for assisting surgeons in clinical decision making.
“From a surgical standpoint, if we can use this algorithm to show how correction with various osteotomies, correcting the spine to a desired sagittal vertical access or restoring PI-LL mismatch, we can then help prevent or reduce the risk of proximal junctional kyphosis,” adds Dr. Lombardi. “We are eager to build models that answer all of the outstanding questions that we have in the spinal deformity world with the ultimate goal of doing better by our patients and improving their outcomes. So many things contribute to the development of PJK and there are things that we as surgeons can control and things that we can’t control. Having a predictive tool for understanding surgical interventions and its role and impact on PJK could be profound.”