In a worldwide first, doctors at NewYork-Presbyterian/Weill Cornell Medicine have developed a technique to treat early breast cancers with MRI-guided prone breast radiotherapy. Their study on the first 11 patients receiving this game-changing treatment, termed “precision prone irradiation” (PPI), appeared in Frontiers in Oncology, November 23, 2022.
With prone breast radiotherapy, the patient lies face down and the affected breast drops down through an opening in the table, allowing radiation oncologists to home in on microscopic cancer cells remaining after surgery while minimizing the collateral damage to nearby organs like the heart and lungs. Up to now, doctors have only been able to use older technologies such as X-ray films or CT scans to guide the delivery of radiation. But the MRI-linear accelerator technology combines the MRI imaging technology and the radiation delivery system to better visualize the surgical site.
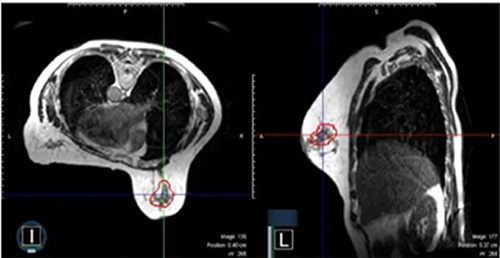
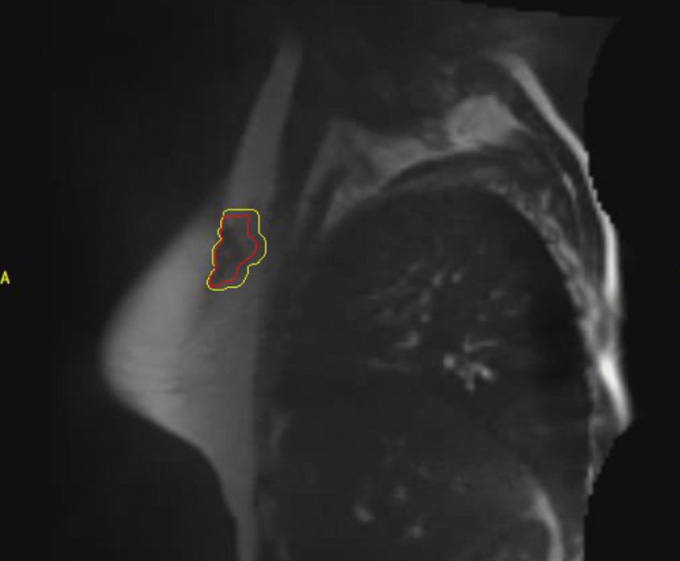
A representative surgical cavity target volume seen from an MRI image acquired on-table on the day of the radiation treatment. The MRI scans in both the axial and sagittal planes are shown. The surgical cavity is outlined in red. (Credit: John Ng, Ryan Pennell and Silvia Formenti. Front. Oncol., 23 November 2022)
PPI is the most advanced breast cancer radiotherapy technique available. By delivering the radiation treatment with MRI-guided precision and also using the prone position, this technology promises to further decrease the amount of normal breast tissue receiving radiation while targeting cancer cells. Currently PPI is available only at NewYork-Presbyterian/Weill Cornell Medicine, one of a limited number of institutions with an MRI linear accelerator, along with a long-standing expertise in breast cancer radiotherapy.
“Ever since there have been radiation treatments for breast cancer patients, the goal has been to improve the technique to better target potential cancer cells and to avoid radiation where it is not supposed to go, most importantly to avoid the heart and lungs,” says John Ng, MD, Assistant Professor of Radiation Oncology at Weill Cornell Medical College and a Radiation Oncologist at NewYork-Presbyterian Hospital and the study’s first author. “Precision prone irradiation continues the ongoing narrative in our field to improve breast radiation techniques to get better outcomes and lessen side effects for our patients.”
The team used the technique for patients diagnosed with ductal carcinoma in situ (DCIS) and early stage cancers treated with lumpectomy, which account for about two thirds of new breast cancer cases. As these patients should receive radiation after breast-conserving surgery as a national standard guideline, PPI could potentially have a significant and broad impact on breast cancer treatment.
A History of Firsts
PPI builds on NewYork-Presbyterian/
Precision Prone Irradiation
“Dr. Formenti started these advances by asking, ‘What if we positioned the patient's body in a more intelligent way so that you can deliver the beams of radiation treatment to avoid the heart and lungs?’” says Dr. Ng. “Now we are widely recognized as one of the global leaders.”
NewYork-Presbyterian/
The technology needed to develop PPI fell into place in 2017, when the FDA approved the MRI linear accelerator. NewYork-Presbyterian/
“When they first came out with the MRI-linear accelerator, the initial focus was in treating abdominal areas or other parts of the body where organs move, the idea being that you wanted to be able to visualize targets and organs in motion,” says Dr. Ng. “But when NewYork-Presbyterian/
By March of 2021, they had it figured out. “The novel part is combining the MRI-guided technique with the prone partial breast radiotherapy technique,” Dr. Ng says. “And we're the first institution and team in the world to do anything like that.”
Calculating the Risks and Benefits
MRI offers significant advantages over the CT scans traditionally used for prone partial breast irradiation. “A CT scan sometimes is not very good at seeing where the tissue changes, meaning that if you look at the breast after surgery with a CT scan, you may not be able to precisely determine where the surgery occurred,” Dr. Ng explains. MRI is better at delineating soft tissue contrast and taking a more detailed picture of the surgical cavity. Also, doing a CT scan entails delivering very low but, nonetheless, safe doses of radiation to the entire body — an MRI scan does not.
The recently published study demonstrated the feasibility of using MRI technology for prone partial breast irradiation and achieved excellent results. The treatments were successfully delivered and the patients only experienced temporary, minimal side effects. Dr. Ng, Dr. Formenti, and Ryan Pennell, PhD, Chief Medical Physicist in Radiation Oncology at NewYork-Presbyterian/
With the pilot study completed and published, the team is now launching a clinical trial in January to see if PPI leads to better disease outcomes or less side effects. The goal is to recruit 400 women with DCIS or early stage breast cancers, favorable tumors less than 2 centimeters in size.
“We're trying to demonstrate that, with the advantages of the MRI technology, we can further decrease the number of treatments for patients, to be able to treat smaller radiation target volumes, and still demonstrate the excellent outcomes that we've come to expect for our patients with favorable risk breast cancers,” says Dr. Ng.
The downside to PPI is that this technology currently takes more resources than delivering radiation using CT imaging, and the treatments take longer. PPI requires the physicians, physicists, and others on the treatment team to be present on each day of treatment to account for any changes on that day.
“We're actually customizing the radiation treatment with each delivery,” says Dr. Ng. “And acquiring an MRI image also requires some time and effort. It's not as straightforward as acquiring a CT image.”
Dr. Ng believes that the challenges of PPI will eventually be resolved. “Because the field itself advances so quickly, I could imagine a time in the near future when this could be done as a standard treatment in hospitals and practices,” he says. “The technologies will get refined and improve over time.”
In the meantime, this novel and advanced technique has drawn attention from radiation oncologists around the world who are curious about bringing it to their centers. NewYork-Presbyterian/
“It’s not too often that you get to say that you were the first team to do something. This is one of those times,” says Dr. Ng. “We’re very proud that we are able to offer this for our patients.”




