Harnessing novel discoveries into the root cause of chronic subdural hematoma and the latest cutting-edge, image-guided cerebrovascular techniques, Jared Knopman, MD, a neurosurgeon and interventional neuroradiologist at NewYork-Presbyterian/
“MMA embolization addresses the unmet need of a growing number of elderly and medically complex patients who are seeking non-surgical treatment for chronic subdural hematoma,” explains Dr. Knopman, Director of Cerebrovascular Surgery and Interventional Neuroradiology at NewYork-Presbyterian/
“This lifesaving treatment, with little surgical risk and excellent outcomes, makes an enormous difference in the patient experience,” says Dr. Knopman. “Embolization is easier than open surgery on patients, especially older ones, and hospitalization time is greatly reduced. Recovery time is much faster. And the risk of infection or other complications is minimized, so it is truly win-win.”
A subdural hematoma develops when blood accumulates under the dura, the outer covering of the brain. It can occur spontaneously or as the result of trauma. “As we age, our brain begins to shrink away from the dura, and we are more prone to having an accident and bleeding in that space,” explains Dr. Knopman, “Even a mild head trauma or jostle can cause veins to tear and a blood clot to form.” In addition to advanced age, other risk factors include taking anticoagulant medications and long-term alcohol use.
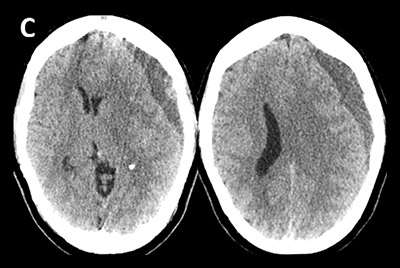
If the blood clot does not resolve, it is considered a chronic or subacute subdural hematoma, which can compress the brain and lead to symptoms including headache, dizziness, cognitive deficits, and neurological deficits. Some small hematomas may be treated with medication, or monitored until they resolve on their own, but larger and symptomatic hematomas usually require treatment.
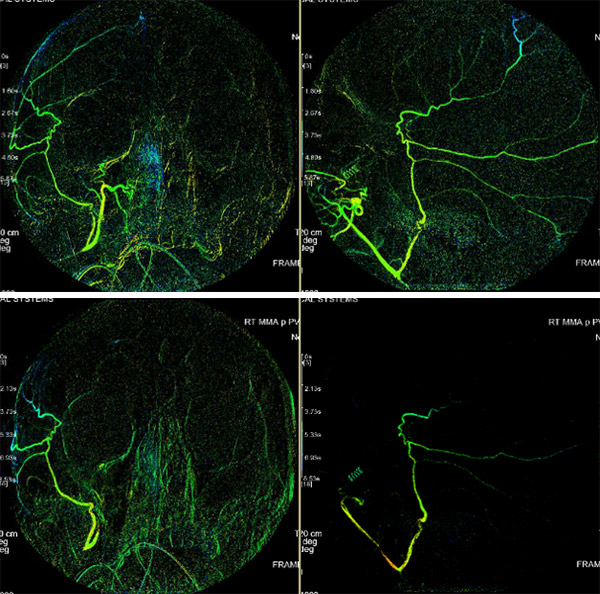
Reconstructed angiograms of a patient who received embolization of the middle meningeal artery; before embolization (above) and after embolization (below)
“For the past 50 years, the mainstay form of treatment has been through burr holes or a craniotomy to remove the hematoma and cauterize the membranes to stop the bleeding,” says Dr. Knopman. “As you can imagine, these procedures are not ideal for patients who are either too elderly or frail to undergo open surgery and general anesthesia, and endure a prolonged recovery.”
Additionally, subdural hematomas are prone to recurrence if the membrane’s blood supply remains intact. “A subdural hematoma can cover half of the skull, and with craniotomy we only open up a small part to drain the blood,” explains Dr. Knopman. “Up to 20 percent of subdural hematomas will recur because these membranes continue to ooze in the area that you can’t shut down. In some studies, as high as 33 percent of patients will require retreatment after evacuation.”
With dual expertise in both open and minimally invasive neurosurgical techniques, Dr. Knopman made a series of groundbreaking discoveries about the root cause of subdural hematoma that raised the possibility of reaching and repairing the hematoma with minimally-invasive interventional techniques instead of open brain surgery. “For half a century, it was thought that subdural hematomas were venous in origin,” explains Dr. Knopman. “Yet when I operated on these clots, I noticed that the hematoma’s membranes were very oozy and friable and had mixed acuity blood products, a combination of old and new blood. Through pathologic and radiographic analysis we could see that the clot forms new arteriole blood vessels that feed from the dura and connect with the MMA, demonstrating an arterial pathogenesis of the subdural hematoma, its growth, and its recurrence.”
“MMA embolization interrupts this blood supply and prevents the rebleeding that keeps the subdural hematoma alive, which then allows the body to resorb the blood and eliminate the blood clot over time,” adds Dr. Knopman. “These blood vessels are pathologic, so they are completely expendable.”
Pre-embolization
Post-embolization
At NewYork-Presbyterian/
Dr. Knopman and his team have since performed more than 350 embolization procedures. “We have achieved a 94 percent success rate in upfront embolization in avoiding or preventing patients from ever progressing to needing surgery,” says Dr. Knopman. “This compares with a roughly 50 percent chance historically in these patients who ultimately needed surgery before MMA embolization. In patients who already need or received surgery because their hematomas were large at the time of diagnosis, we have a five percent recurrence rate among patients who need a follow-up re-evacuation after embolization compared to 20-30 percent recurrence rates after surgery alone.”
“The key benefit to MMA embolization is that it doesn’t take off the table the potential for surgery if it doesn’t work, but it offers an upfront alternative to surgery if it does work,” he adds. “The procedure is low risk, you’re able to avoid surgery, but if it doesn’t work, we’re right back to where we’ve been always for the treatment of this disease, which is surgery.”
NewYork-Presbyterian/
“The EMBOLISE trial is expected to solidify MMA embolization as the standard of care for chronic subdural hematoma across the world,” says Dr. Knopman, who serves as Principal Investigator. “EMBOLISE will help us optimize the technique and determine what constitutes success for embolization from a radiographic and clinical standpoint.” The study is expected to be completed by 2024.
“MMA embolization is a sea change in how we’re treating patients with chronic subdural hematoma, which is largely a patient population that is elderly and fragile,” says Dr. Knopman. “However, any person with a chronic hematoma is a potential candidate for the procedure. This includes those patients that don’t need immediate surgery, as well as those that do. We are now offering this technique to our most challenging patients who previously were unable or contraindicated to ever receiving surgery – those on blood thinners or those who have very low platelets due to leukemia or an oncologic disorder.”
Dr. Knopman’s expertise is widely sought and he serves as a mentor to neurosurgeons at centers across the country. “MMA embolization has been the most professionally satisfying thing I’ve ever done,” he says. “I get calls from neurosurgeons who are learning how to do it for their patients. They follow up with me and say the procedure was a success, and they’ve saved their patients. It’s wonderful to hear stories about people I’ve never met, yet I can make such a difference in their longevity and quality of life.”