Dr. Roger Härtl
For nearly 20 years,
In an effort to eliminate this disruption and streamline image-guided spinal surgery, Dr. Härtl and his neurosurgical colleagues at NewYork-Presbyterian/
“Augmented reality enables us to color code each structure that we are looking for,” explains Dr. Härtl. “We have used this approach for tumors because as defined structures inside the spine they can be outlined and then visualized in color. With augmented reality, you can see the structure through your surgical glasses or through a microscope, an endoscope, or exoscope without having to introduce the pointer instrument. The AR technology helps surgeons identify crucial landmarks more quickly and with greater accuracy, especially in patients with complex anatomy or in revision cases. But the point is that AR can be applied to any structure relevant for the surgery and that's what we did with transforaminal lumbar interbody fusion [TLIF].”
The AR technology helps surgeons identify crucial landmarks more quickly and with greater accuracy, especially in patients with complex anatomy or in revision cases.
— Dr. Roger Härtl
The neurological surgery faculty at Weill Cornell Medicine recently completed two studies that confirmed the feasibility and utility of incorporating augmented reality into spine surgery. One study looked at the role of AR in improving surgical workflow and eliminating fluoroscopy in MIS-TLIF. The second study evaluated the application of AR in minimally invasive and open resection of benign intradural extramedullary tumors. Findings of both studies were published in the September 2022 issue of Neurospine.
Facilitating Workflow in MIS-TLIF
Transforaminal lumbar interbody fusion is a well-established surgical procedure to stabilize and decompress a spinal motion segment using a unilateral facetectomy to access the disc space in order to implant a cage and/or bone graft. TLIF is routinely performed through traditional open or minimally invasive techniques and is associated with excellent outcomes. Dr. Härtl and his colleagues have found augmented reality to be particularly suited for use in this procedure to delineate sequential surgical landmarks.
“AR allows you to highlight any structure that is relevant for the surgery,” says Dr. Härtl. “The TLIF procedure is a minimally invasive spinal fusion procedure for patients with conditions such as spondylosis, which can cause severe nerve compression and spinal instability. The operation is characterized by a consistent sequence of key surgical steps that always include specific bony landmarks – lamina, pars interarticularis, facet joint, inferior pedicle, and superior pedicle – relevant for the surgery. As a surgeon, you look for these surgical landmarks.”
Prior to surgery, Dr. Härtl color codes each of these bony landmarks. “During surgery, I look for the first surgical landmark, which is the lamina, click on the button and then through the microscope I can see the lamina in the color that I highlighted before surgery. Now I know exactly where to go because I can clearly see landmark number one.”
As Dr. Härtl describes, the surgeon continues moving on to each landmark sequentially through the click of a button. Likewise, when the landmark is no longer needed, it can be turned off just as easily. “Essentially, this streamlines the procedure by guiding the surgeon from one landmark to the next minimizing the risk of omitting a surgical step.”
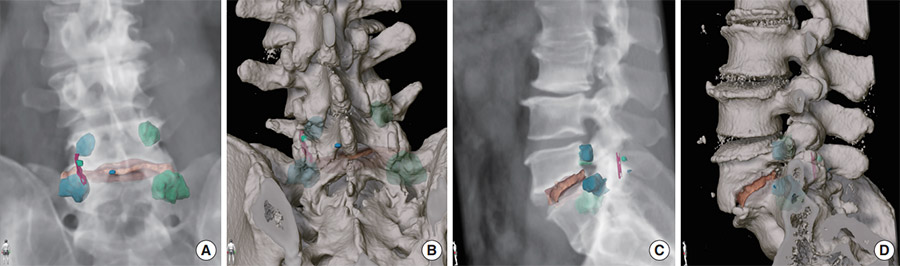
Landmarks for a L5/S1 transforaminal lumbar interbody fusion via left sided surgical approach highlighted on a CT 3D reconstruction posterior view (A, B) and left sided lateral view (C, D). (Credit: Neurospine, September 2022)
In the images above, L5 inferior medial edge of the lamina is indicated in blue; L5 pars, green; L5/S1 superficial facet joint space, purple; S1 “pedicle” ipsilateral, light blue; L5 pedicle ipsilateral, light blue; L5/S1 posterior part disc space, orange; and L5 and S1 pedicle contralateral, light green.
In their study of AR utilized for MIS-TLIF, the research team at Weill Cornell Medicine developed and evaluated a protocol to integrate AR into the surgical workflow conducting a case series of 10 patients serving as the basis for the evaluation. Surgical TLIF landmarks, which included anatomic landmarks and screw trajectories for the posterior instrumentation, were marked on a preoperative CT scan that was then fused intraoperatively with the low-dose navigation CT scan to which the markers were transferred.
The study demonstrated several potential benefits of integrating augmented reality in MIS-TLIF:
- Planning of the procedure can take place in advance as part of the regular preoperative review of radiological imaging and does not delay the duration of the procedure.
- While the use of AR requires two additional steps – the fusion of the preoperative planning CT with the intraoperative navigation CT and the calibration of the microscope to the navigation system – the image fusion is performed using the same hardware used for navigation, eliminating the need for an additional device in the OR.
- The image fusion and calculations are performed in a manner that does not interrupt the use of the navigation feature of the device, essentially resulting in no delay in the surgical procedure.
“The MIS-TLIF procedure is particularly suitable to be supported by AR, as it is a procedure that is highly reliant on accurately recognizing anatomic landmarks,” note the authors.
Optimizing Intraoperative Tumor Localization
“For some time the concept of color coding has been applied to surgery to remove spine tumors because a tumor presents an obvious target,” says Dr. Härtl. “Using stereotactic navigation, you can visualize the spinal tumor before you make a skin incision. You know exactly where to go with your incision, how big the incision has to be, and at which level and on which side. Traditionally, we have used this for tumors because those are defined structures inside the spine that you can outline and then visualize in color code. But with augmented reality, you would be able to see the tumor through your surgical glasses or through the microscope.”
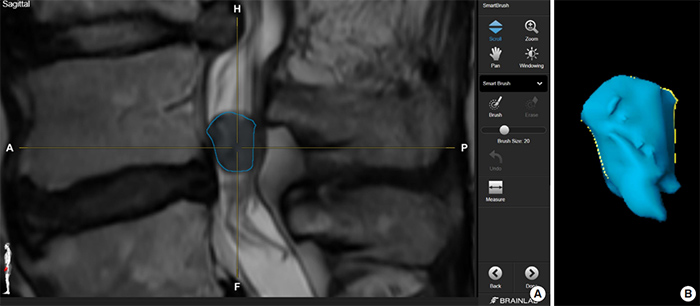
(A) Highlighting of the neoplasm on a preoperative MRI software (B) “Smartbrush” function of the software automatically renders the 2-dimensional highlighting on the MRI into a 3-dimensional shape (Credit: Neurospine, September 2022)
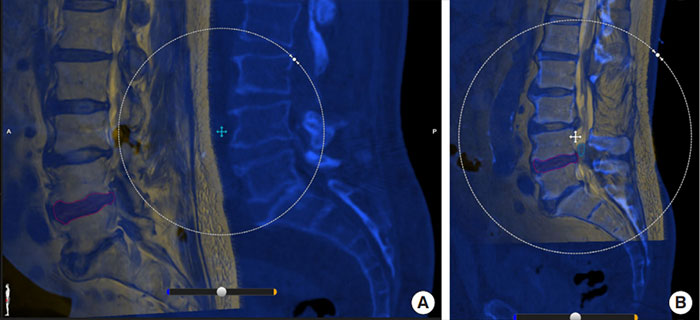
(A) Elastic image fusion of the preoperative planning MRI scan (yellow) and the intraoperative navigation CT scan (blue). (B) The scans are manually calibrated to be most accurate on the level closest to the surgical site. (Credit: Neurospine, September 2022)
Dr. Härtl and his neurosurgical colleagues conducted a case series demonstrating how augmented reality can be safely applied to tubular minimally invasive and open resection of benign intradural extramedullary tumors and allow for intraoperative localization of a tumor from skin through the intradural compartment.
Similar to their study of AR application to MIS-TLIF, the team developed a protocol for spine tumors in which the tumor is marked on diagnostic magnetic resonance imaging (MRI) using AR software and then fused intraoperatively with the low-dose computed tomography. The authors note the position and size of the tumor is projected into the surgical microscope and directly into the surgeon’s field of view and orientation is performed exclusively via navigation and AR projection. “For spinal tumor surgery, this technology can be particularly helpful in minimizing injury to the surrounding soft tissues by guiding the surgeon from the beginning of the surgery during incision planning and tubular insertion trajectory,” explains Dr. Härtl.
This study, to our knowledge, is the first study on AR-assisted minimally invasive resection of benign intradural extramedullary tumors involving the lumbar spine.
— Dr. Roger Härtl et al, Neurospine, September 2022
The researchers evaluated the clinical feasibility of AR-assisted resection in a prospective case study of eight consecutive patients between November 2020 and August 2021. Their case series revealed:
- AR integration into the regular surgical procedure was efficient as the image fusion can be performed in parallel with the other surgical steps and did not interrupt the workflow nor cause any delay of the surgical procedure.
- Accuracy of projecting the AR into the microscope corresponded exactly to the position of the tumor in all cases.
- In one case of a tumor with an irregular shape and extension of the tumor into the neuroforamen, AR-guidance was key to achieving gross total resection.
- Opening the dura did not result in any relevant inaccuracy of the AR projection and was always performed at the level of the AR projection and corresponded to the actual position of the tumor in all cases.
- After resection of the tumor, AR was found helpful in the lumbar spine to inspect the resection site for any residual tissue before closing.
The authors concluded that the use of AR in detecting spinal tumors is a “safe and effective alternative or adjunct to existing intraoperative orientation methods, such as ultrasound, particularly for minimally invasive approaches.”
“While there are many promising applications for augmented reality in the surgical arena, in our experience we estimate a learning curve of about 10 cases in which surgeons can become familiar with the technology, planning software, and workflow steps,” advises Dr. Härtl. “Augmented reality is also an excellent teaching tool when used on anatomical training models and in live surgery with the potential to assist in illustrating a complex surgical procedure and facilitating teaching and training. Importantly, AR is a surgical tool for experienced surgeons to safely facilitate surgery in patients with complex anatomy, those who have had previous surgery resulting in scar tissue, or patients with degenerated spine and very complicated anatomy. There are so many different facets of surgical navigation and we tend to focus on one versus the other. At the end of the day, we should take advantage of each of these approaches in combination to truly benefit from navigation technologies.”