Timothy C. Wang, MD, is Chief of the Division of Digestive and Liver Diseases at NewYork-Presbyterian/
These leadership appointments speak to Dr. Wang’s renowned and enduring reputation as a pioneering clinician-scientist in gastroenterology cancer. His laboratory has long investigated the molecular mechanisms of gastrointestinal carcinogenesis supported with decades of continuous funding by the National Institutes of Health and the National Cancer Institute. In March 2022, in recognition of his lifelong contributions to the field of gastroenterology, the American Gastroenterological Association recognized Dr. Wang with its highest honor, the Julius Friedenwald Medal.

Dr. Timothy Wang
“Our laboratory has been studying stomach cancer for more than 30 years, focused initially on the role of Helicobacter pylori infection as an initiating and promoting factor,” says Dr. Wang. “In collaboration with MIT, we helped to develop the first Helicobacter-dependent mouse models of gastric cancer and discovered the key role of chronic inflammation in driving gastric carcinogenesis. Our faculty have gone on to develop multiple models of gastric cancer, which allowed us to uncover the stem cell origins of both metaplasia and cancer.”
During the past five years, supported by a multi-year grant awarded by the NCI, Dr. Wang and his Columbia colleagues have been investigating the role of nerve and other stromal cells in the development of digestive cancers. The research builds on earlier studies in which they advanced the premise that by inhibiting stromal cells in the microenvironment, it may be possible to inhibit the development of tumors. The researchers are calling on a large collection of genetically engineered mouse models and in vitro 3D organoid cell models to better understand the normal stem cell niche and the alterations that occur in the cancer cell niche that presumably contribute to tumor progression.
In the August 5, 2021 issue of Cell Stem Cell, the Columbia researchers discuss the biology of gastroesophageal stem cells, their role as cells of origin in cancer, and interactions between the stromal niche and gastroesophageal stem cells in metaplasia and early expansion of mutated stem-cell-derived clones during carcinogenesis.
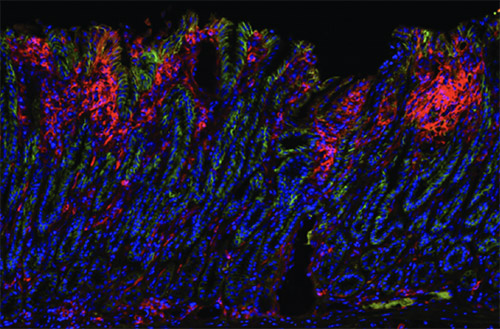
Stomach cancer cells from a mouse model (Courtesy of the Wang Lab)
Growing evidence from studies of human derived cells and mouse models supports a gastric origin of esophageal adenocarcinoma and Barrett’s esophagus in that their pathogenesis involves the aberrant differentiation of stem or progenitor cells at the gastroesophageal junction. This unique transitional zone contains actively dividing epithelial stem cells that with prolonged inflammation can transition to intestinal metaplasia and enable a predisposition to cancer.
According to the Columbia research team, while the stomach and esophagus belong to the same functional unit, they contain “distinct stem and progenitor cell populations needed to sustain rapid cellular turnover.” Detrimental conditions, such as bile acid reflux and H. pylori infection, can cause an abnormal differentiation of gastric progenitor cells that, in turn, leads to a mixture of cells with gastric and intestinal differentiation in the squamous-columnar junction or stomach and an increased cancer risk.
Columbia faculty have developed multiple models of gastric cancer, which allowed researchers to uncover the stem cell origins of both metaplasia and cancer.
While innovative models of metaplasia and cancer have introduced new cell-of-origin and molecular mechanisms in gastric cancers, novel cell populations have been identified in the upper GI tract, uncovering challenges that are multipronged:
- None of the markers identified thus far have been specific for distinct stem cells and may overlap with the same stem cell population.
- Most of the markers have not been confirmed in human tissues.
- Heterogeneity of marker-positive populations has been underestimated.
- Newer approaches are needed to determine whether a homogeneous single progenitor model or a heterogeneous/hierarchical model exists that defines the upper GI tract.
For the past decade, in vitro growth of gastric or esophageal organoids in 3D culture has been used for stem cell research. In recent years, producing 3D organoid cultures in Matrigel using gastric or esophageal tissue from affected individuals has been gaining attention. With this approach, primary cultures from surgical specimens, endoscopic biopsies, or through induced pluripotent stem cells (iPSCs) are differentiated into gastric or esophageal tissue. PSC-derived human gastric organoids not only provide the ability to grow gastric epithelial progenitors in conjunction with a stromal niche, these models can be used to better understand human gastric stem cells and the critical interactions with distinct cell types such as endothelial, neuronal, immune, mesenchymal, and other niche cells.
“Changes in these niche cells lead to expansion of stem/progenitor cells, as well as suppression of tumor immunity, allowing for progression to dysplasia and cancer,” explains Dr. Wang. “Even with advances that confirm stem cells play a central role in mucosal homeostasis and are the primary source of metaplasia and cancer in the esophagus and stomach, numerous questions remain.”
The marked heterogeneity in presumed esophageal and gastric stem/progenitor cell populations remains an important line of inquiry for the Columbia researchers. Based on experience in the hematopoietic stem cell field, identifying a highly specific stem cell marker will be difficult. Additional methods for sorting and sequencing individual stem cell subpopulations and defining functional characteristics need to be created.
The researchers note that cellular plasticity also remains an open question. While the degree of plasticity by differentiated cells is likely overestimated, mechanisms are in place to restore homeostasis following injury or loss of dedicated stem cells. Although plasticity can be studied for its role in tissue regeneration, the potential for dedifferentiation or interconversion from progenitor cell types may present challenges when targeting stem cells and/or cancer stem cells for cancer therapy.
The authors conclude, improving “understanding of signaling pathways that activate stem cell function, the niche components that generate the signals, and the mechanisms for cellular interconversion or dedifferentiation processes are exciting areas for future study.”



