An estimated 100 million Americans have some form of non-alcoholic fatty liver disease (NAFLD). Considered uncommon 30 years ago, the prevalence of NAFLD has been increasing in parallel with the rising obesity rate. NAFLD can be reversed with weight loss, but there are few if any treatments available to reduce or stop the progression of fibrosis, which can lead to liver failure or cancer.
Research by Columbia and Weill Cornell gastroenterology faculty continue to advance understanding of the biological mechanisms of non-alcoholic fatty liver disease and best practices for its management.
Manifestations of NAFLD Beyond the Liver
NAFLD is strongly associated with the metabolic syndrome but can occur independently of existing metabolic diseases. In addition to liver-related disease and associated mortality, other significant outcomes can include cardiovascular diseases, chronic kidney disease, and type 2 diabetes. Columbia transplant hepatologist Julia Wattacheril, MD, MPH, sheds light on these extrahepatic manifestations in the March 2020 issue of Gastroenterology Clinics of North America. Dr. Wattacheril emphasizes the significance of interventions that focus on monitoring progression of liver disease, while at the same time addressing overall morbidity and mortality from other organ systems.
Regulating Biological Activity in NAFLD
The liver plays an essential role in maintaining whole-body lipid and glucose homeostasis, which is primarily mediated by the transcriptional activation of hepatic pathways that promote glucose and lipid production or utilization in response to the nutritional state of the body. In addition to activation of inflammatory and fibrogenic pathways in the liver, obesity often results in the dysregulation of lipid and glucose metabolism and is therefore the primary risk factor for the pathogenesis of metabolic disorders. Transcription factors that are associated with obesity-induced liver injury and the pathogenesis and progression of NAFLD often serve essential biological functions in the maintenance of energy homeostasis and stress response.
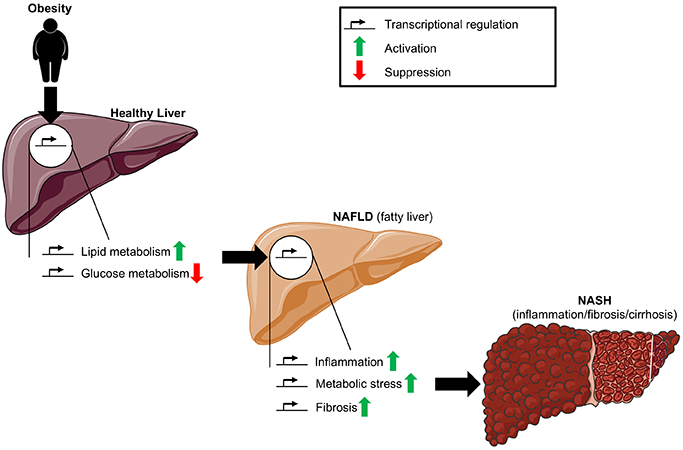
Diagram displaying how to manage fatty liver disease.
In an article published in the July 9, 2020 issue of Metabolites, Weill Cornell faculty provide a comprehensive review of their current understanding of the transcription factors involved in the pathogenesis and progression of NAFLD, with a focus on lipid and glucose metabolism, inflammation, metabolic stress, fibrosis, and the gut microbiome. They also address the relevance of mouse models to human pathophysiology. The authors note that novel experimental models that more accurately reproduce human pathophysiology, including mice with humanized livers, will be central to the discovery of amenable targets for the management of NAFLD.
Benefits of Endoscopic Sleeve Gastroplasty for NAFLD
Weill Cornell gastroenterology faculty are evaluating the role of endoscopic sleeve gastroplasty (ESG), a promising procedure for treatment of obesity, and its benefits related to insulin resistance, hepatic steatosis, and fibrosis in patients with NAFLD. Their study followed for two years 118 patients with obesity and NAFLD who underwent ESG. The results, published in the August 27, 2020 issue of Gastrointestinal Endoscopy, showed:
- Mean total body weight loss was 15.5 percent
- HOMA-IR (homeostasis model assessment of insulin resistance) significantly improved from 6.7±11 to 3.0±1.6 after only one week, with continued improvement up to two years
- HSI (hepatic steatosis index) score significantly improved, decreasing by 4 points per year
- NAFLD fibrosis score significantly improved, decreasing by 0.3 point per year
- 24 patients (20 percent) improved their risk of hepatic fibrosis from F3-F4 or indeterminate to F0-F2; only 1 patient experienced an increase in the estimated risk of fibrosis
This data suggest that ESG produces a significant and sustained improvement in estimated hepatic steatosis and fibrosis in patients with NAFLD. Importantly, the study revealed an early and weight-independent improvement in insulin resistance, which endured for two years following ESG.
Understanding NAFLD in Non-Obese Individuals
The pathophysiology and risk factors for the development of NAFLD in non-obese persons are not fully understood. They seem to be closely associated with insulin resistance; elevated levels of triglycerides, small-dense low-density lipoprotein, and low levels of high-density lipoprotein cholesterol; and alterations in body composition, with some patients who may have a predisposition to genetic polymorphisms. Individuals with NAFLD who do not have the typical risk factors may also develop non-alcoholic steatohepatitis (NASH) and progression to more advanced liver disease.
In lean individuals, lifestyle change for disease management has limited potential. In the December 13, 2019 issue of Frontline Gastroenterology, Columbia hepatologists discuss the clinical, histological, and genetic features and risk factors for non-obese NAFLD and highlight areas for future research, including biological mechanisms that may identify novel targets for intervention in this population. This cohort represents one phenotype of interest currently undergoing whole exome sequencing and analysis as part of Columbia’s precision medicine initiative.



