Physicians at NewYork-Presbyterian/Weill Cornell Medicine’s Comprehensive Weight Control Center (CWCC) have long been at the forefront of research of anti-obesity medications (AOMs), a category that continues to grow in response to the increasing prevalence of obesity among U.S. adults. With the advent of combinations such as phentermine/topiramate and naltrexone/bupropion, as well as single-agent glucagon-like peptide-1 (GLP-1) receptor agonists such as liraglutide, individuals could potentially lose between 5% to 10% of their body weight, according to Alpana Shukla, MD, a NewYork-Presbyterian/Weill Cornell Medicine physician and Director of Clinical Research at the CWCC.
The use of GLP-1 agonists, originally developed to treat diabetes mellitus, has gained traction as more effective agents, such as semaglutide, yield average weight loss of 15% and about a third of individuals can lose 20% of their weight. The category appears to remain on an upward trajectory, as reflected in the recent approval of the dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 agonist tirzepatide, which reportedly pushes average weight loss to 21% and over a third of patients can experience 25% or more weight loss.
The availability of highly effective AOMs makes this “a very exciting era,” says Dr. Shukla. “You could say that we are closing the gap between the kind of results you will get from treating patients with medication versus the kind of outcomes you would get from doing bariatric surgery, which I think is a huge advance in the field.”
We are closing the gap between the kind of results you will get from treating patients with medication versus the kind of outcomes you would get from doing bariatric surgery, which I think is a huge advance in the field.
— Dr. Alpana Shukla
Nevertheless, widespread uptake of the newer, more effective AOMs has been limited by their high cost, insurance coverage exclusions, and lack of treatment persistence. Moreover, “there is a huge knowledge gap in our field because until recently, we didn’t know how people do in terms of weight loss outcomes beyond one year,” Dr. Shukla notes, adding that most clinical trials have been of one-year duration, with some lasting as long as two years. Consequently, long-term outcomes in the literature have generally been reported at 12-18 months. “It’s important for us to know how people actually do in the long term because obesity is a chronic disease, just like hypertension and diabetes,” she comments. “That’s why we drew upon the rich patient experience at the Comprehensive Weight Control Center to fill the knowledge gap that exists in the literature.”
Reviewing the Use of AOMs Over a Five-Year Period
Dr. Shukla and colleagues conducted a retrospective observational study of 428 adults with overweight or obesity who were treated with FDA-approved and off-label AOMs at the CWCC. The five-year study results were recently published in The Journal of Clinical Endocrinology & Metabolism.
“The impetus of the study was to examine our own patient cohort and understand how people are doing long-term,” Dr. Shukla explains. “It’s a question that often comes up in practice as well. Sometimes I would like to be able to tell my patients what they can expect if they keep following up. We also wanted to understand the safety aspects of how we were treating our patients. Were there any things we could have been doing differently? What were the factors associated with some patients doing better than others?”
Patients were eligible for the study if they had an initial visit between April 1, 2014, and April 1, 2016, and had follow-up of six months or more. Average weight loss from initial to final visit – the study’s primary endpoint – was 10.4% at a mean follow-up duration of 4.4 years. The proportions of patients who met the weight reduction targets of 5% or greater, 10% or greater, 15% or greater, and 20% or greater were 70.8%, 48.1%, 29.9%, and 17.1%, respectively. Those results were “in the range of what I think we expected,” notes Dr. Shukla. She describes the 10% or greater weight loss at five years as “a good result because we know that is an amount of weight loss that actually has important health benefits. The goal is not just to lose weight; weight’s a number. The question is, what does that weight loss do to you? How does it improve your blood pressure? How does it reduce your risk of diabetes?”
On average, the patients regained 51% of their maximum weight loss, while 40.2% of patients maintained their weight loss. “We were happy and pleasantly surprised to see that a third of them actually maintained 15% or more, which I think is very significant,” Dr. Shukla observes. Her group previously conducted a study in which weight-loss outcomes at two years were similar to those at one year. “If you think about it, if people are with you for two years and they’ve maintained that weight loss, the likelihood of them keeping that weight off long-term is pretty good.”
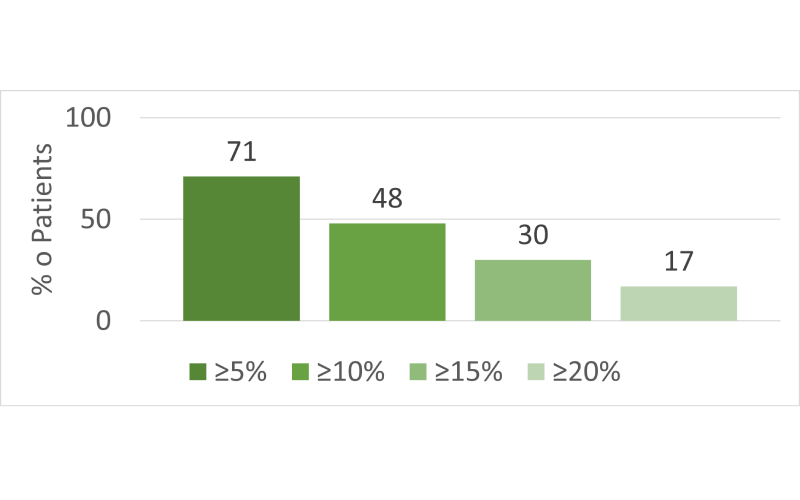
Half of patients achieved and maintained ≥10% weight loss.
On the other hand, the weight regain results did not surprise Dr. Shukla. “When people do lifestyle interventions, you’ll see that they regain over time. Half the people at five years have regained all the way. And the ones who actually keep weight off, on average, regain 80% of the weight they’ve lost. In our cohort, patients regained about half of the weight they lost, on average. I would’ve hoped that this could have been better, but this is in line with what I would expect. Even people who have bariatric surgery regain some weight. This is expected because we know that the body’s intrinsic hormonal and energy-regulating mechanisms adapt in response to weight loss, which promotes weight regain. This is why we say obesity is a chronic relapsing disease.”
“That’s why people need to keep following up because there may be a need for adjustment of therapy,” Dr. Shukla continues. “And that’s what we found: people who actually followed up more consistently, or had more interactions with their providers, which afforded maybe an opportunity to tweak their treatments, actually had more success.” She notes that multivariable regression analysis showed a higher number of clinic visits remained statistically significantly associated with 10% or greater weight loss (odds ratio [OR] 1.04; P = .002). Each additional clinic visit was associated with a weight reduction of 0.17%.
Which AOMs Were Used Most Frequently and Consistently?
Metformin (88.3%), topiramate (44.2%), phentermine (42.1%), and bupropion (29.4%) were the most common medications trialed in the study. At the final visit, the most commonly used AOMs, alone or in combination, were metformin (73.6%), phentermine (28.0%), topiramate (27.6%), bupropion (25.7%), and semaglutide (14.3%). Metformin, topiramate, and bupropion were associated with increased odds of maintaining 10% or greater weight loss. Whereas a mean of 4.3 AOMs per patient were trialed over the study period, at the final visit patients were taking a mean of 2.1 AOMs, and 65% were taking two or more.
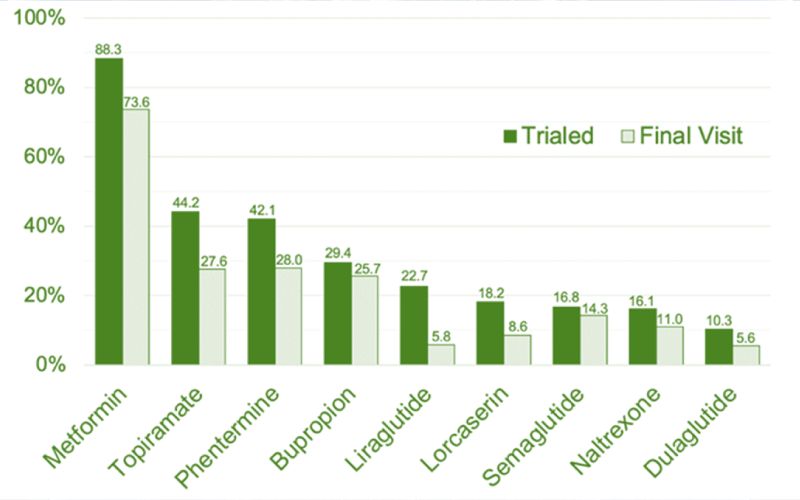
Metformin, topiramate, and phentermine were the most commonly prescribed AOMs in this cohort.
Dr. Shukla notes that the study cohort was established before the introduction of many currently available AOMs. Whereas semaglutide was available toward the latter part of the study period, the average dose used during the study period was 0.5 mg, which is much smaller than the weight-loss dose (2.4 mg). “The majority of our patients were actually using off-label medications, primarily due to access issues because the insurances don’t often cover the branded medications.”
Nevertheless, “because this is retrospective, there are certain limitations in interpreting these data because you only know what happens to people who follow up,” Dr. Shukla cautions. “We don’t know what happens to people who don’t follow up. But I would say that even given that caveat, it’s clear that these drugs were well tolerated and effective in the patient cohort, because it’s really a reflection of our clinical practice of tailoring treatment to the individual patient.”
NewYork-Presbyterian’s Innovative Approach to Weight Loss
Dr. Shukla highlights the importance of shared decision-making between provider and patient in choosing medication based on patient preference, presence of comorbidities, safety, and other factors. Such considerations are characteristic of the CWCC’s approach to treating patients, which recognizes “the complexity of the disease and that there are multiple pathways” that contribute to the pathogenesis and persistence of obesity. The center is also known for combining medications, an approach pioneered by Louis J. Aronne, MD, director of the NewYork-Presbyterian/Weill Cornell Medicine’s CWCC and one of the study’s co-investigators. The effectiveness of the polypharmacy approach has spurred its adoption by other obesity research centers, “but clearly we have been leading the way in this,” Dr. Shukla says.
Looking to the Future of Weight Loss Management
“We’re at the stage where we know that we have highly effective medications, with the next generation of anti-obesity medications just around the corner,” Dr. Shukla remarks. “The next step for us is thinking more carefully about preserving muscle mass while people are losing weight. I think a lot of the research is going to look at how the combination of medications can help preserve muscle mass and body composition, and how that is going to tie into long-term health outcomes.”
Speaking of long-term outcomes, the salutary effects of AOMs – i.e., in addition to weight loss – will surely be a key focus for the future. Dr. Shukla describes the recently announced results from the SELECT trial, in which semaglutide reduced the composite endpoint of death from cardiovascular (CV) causes, nonfatal myocardial infarction, or nonfatal stroke by 20% in individuals with preexisting CV disease, as “the best news for the field of obesity medicine. I think it’s now time that people have recognized that what we’re treating is a disease. It’s not just about becoming skinny; it’s really about improving health and making people live longer. In the future, we’re going to see more research into these areas, looking at the impact of medications on those sorts of endpoints.”



