Wireless Stimulation: No Leads Required
Cardiac resynchronization therapy (CRT) is a lifesaving procedure to treat arrhythmias in patients with heart failure. However, about 30 percent of heart failure patients receiving conventional CRT do not respond to the treatment, and approximately 5 to 10 percent of these patients cannot be implanted with left ventricular leads because their vessels are too small, unable to be cannulated, located near the phrenic nerve, which should not be stimulated, or in areas that require too much energy to stimulate. In these cases, the only treatment option is open-heart surgery in which the lead is placed on the outside of the heart.
Weill Cornell Medicine faculty are participating in the international, multicenter, randomized SOLVE CRT trial of the WiSE-CRT System, a device that offers a new way to pace the left side of the heart without using pacing leads in patients with poor therapeutic alternatives. The wireless cardiac stimulation system for the left ventricle is intended to help reduce certain complications associated with traditional CRT devices. Candidates for the clinical trial include patients who have had CRT without improving their condition or CRT was attempted to be implanted without success.
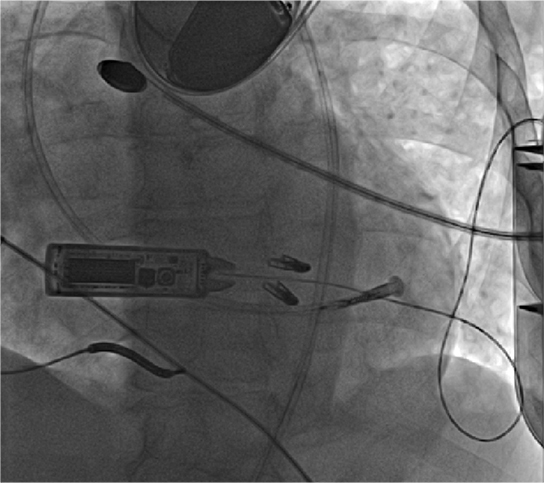
WiSE™ CRT System wirelessly transmits ultrasound energy to a receiver electrode implanted inside the left ventricle. (Courtesy of Weill Cornell Electrophysiology)
The WiSE-CRT System (wireless simulation of the endocardium) consists of a receiver electrode and an ultrasound transmitter. The tiny wireless electrode about the size of a grain of rice is implanted directly inside the left ventricle and stimulated by an ultrasound transducer implanted underneath the skin in the left chest. Participating patients will have either an existing pacemaker or defibrillator that paces the right side of the heart. The transducer will detect that stimulation from the right side of the heart and then send an ultrasound beam to the electrode, which is sitting in the left side of the heart. Resynchronization is achieved within a fraction of a second without the use of pacing leads. This approach also provides cardiologists with a greater choice of pacing locations, thereby enabling patient-specific customization of the pacing site
The study will determine if the combination of endocardial pacing and patient-specific electrode positioning is effective for the population of patients who did not have a response to the standard CRT approach or whose heart failure symptoms did not improve due to device factors, for example, the way in which the traditional lead is positioned or because the heart is being stimulated from the outside rather than from the inside. Having the flexibility to place the electrode in various locations within the heart may improve their response rate.
The study is expected to enroll 350 heart failure patients who have failed to respond to, or are otherwise unable to receive, conventional cardiac resynchronization therapy.
ICD Therapy: Shock Resistance
Patients with Tetralogy of Fallot (TOF) are at increased risk for sudden cardiac death, often undergo implantable cardioverter defibrillator (ICD) implantation at younger ages, and are at greater risk of experiencing inappropriate shocks. However, while the increased rates of inappropriate ICD therapy in these patients have been reported on, other data about the nature of the shocks was scarce.
In a 20-year retrospective review of 44 patients with repaired TOF and ICD implantation, Columbia researchers looked at the prevalence of inappropriate shocks, their characteristics, and follow-up therapeutic interventions. They found that 11 (25 percent) patients with ICDs experienced inappropriate shock therapy, usually occurring within the first two years after implant or years later. Of these 11 patients, 3 received shocks for sinus tachycardia, 7 patients for atrial arrhythmias with rapid ventricular response, and 1 patient was shocked due to noise artifact inappropriately sensed as ventricular fibrillation.
Among the authors’ conclusions:
- Approximately 1 in 4 patients with a history of repaired TOF and ICDs are at risk of experiencing inappropriate shock therapy from their ICDs, which is similar to other findings regarding the rates of inappropriate shocks among patients with congenital heart disease
- Major reasons for inappropriate shocks included supraventricular tachycardia and lead malfunction
- Timing of inappropriate shocks tended to cluster either within the first two years after device implant or generator change, or more than 8 years afterward, suggesting that inappropriate therapy may be related either to suboptimal programming at implant/generator change or to atrial arrhythmia or device malfunction as the patient and ICD system age
- A lower ventricular tachycardia therapy zone was associated with more inappropriate shocks in repaired TOF patients with ICDs
- Strategies that include effective atrioventricular nodal blocking agents for rate control, antiarrhythmic medications, and/or catheter ablation are effective tools to prevent inappropriate ICD shock therapy
Catheter Ablation: Advantageous for AT
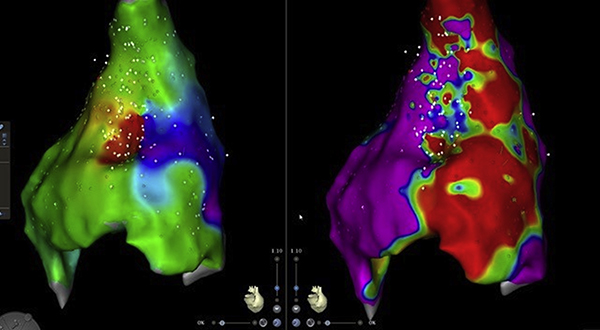
Perivalvar re-entrant tachycardia in a patient with congenitally corrected transposition of great arteries with ventricular septal defect and pulmonic stenosis. Catheter ablation of incisional atrial tachycardia. The activation sequence map (left panel) and the voltage map (right panel) of the posterior right atrium are shown. There is heavy scarring (red zone) from previous surgeries and there is a critical isthmus in the scarred zone. (Source: JACC: Clinical Electrophysiology, April 2019)
Columbia researchers also reported on a retrospective review of the outcomes of 140 patients undergoing catheter ablation for the treatment of atrial tachycardia (AT), determining that catheter ablation in patients with adult congenital heart disease is effective in controlling arrhythmias. Specifically, acute procedural success was a predictor of freedom from recurrence, and the majority of patients achieved multiple arrhythmia-free years. The authors note that common among the patients were multiple arrhythmia mechanisms and latent recurrences requiring repeat procedures. While elimination of all spontaneous and electrically induced atrial tachycardia may be challenging, it appears necessary for durable AT-free survival.



