Infections are among the most serious complications of cardiac implantable electronic devices (CIED), and the rate of infections continues to increase – even outpacing the rate of CIED therapy. According to the American Heart Association’s National CIED Infection Initiative, as many as 1 in 20 patients with a CIED develops an infection within three years of implantation. “If patients with devices who have systemic infections and endocarditis are not managed appropriately, the mortality rate is very high,” says Jim W. Cheung, MD, a cardiac electrophysiologist, Professor of Medicine and Director of Clinical Electrophysiology Research at NewYork-Presbyterian/Weill Cornell Medicine. “Despite these dire consequences, the recognized treatment consisting of removal of the device and all its components remains woefully underutilized.”
With their own clinical experience and observations that many patients with systemic infections were being undermanaged by not having lead extraction or the device system removed, Dr. Cheung and his Weill Cornell Medicine colleagues wanted to determine the actual scope of underutilization in the real world.
“According to the 2017 Heart Rhythm Society guidelines, endocarditis in a patient with a cardiac implantable device is a Class 1 indication for complete system removal,” continues Dr. Cheung. “Even though this has been an indication for more than five years, internal medicine physicians and those in other specialties may not be aware of the guidelines because they do not routinely see these types of cases in their practice. In our own clinical practice, we have seen patients with device-associated infections who have been transferred to us from other hospitals that have had a prior history of relapsing infections over years. In these cases, the failure to recognize that complete device removal is required for complete clearance of infection led to unnecessary recurrent hospitalizations. Based on these observations, we hypothesized that is an under-appreciation in the community of the need for device system removal to adequately treat patients with pacemakers and defibrillators who have systemic infections.”
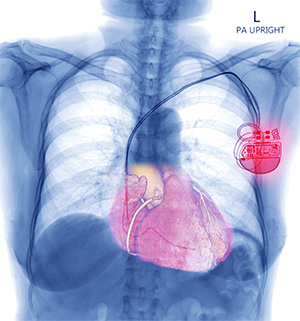
X-ray image showing a CIED
“In general, when a patient develops a systemic infection, a 4–6-week intravenous antibiotic course will be sufficient to treat the infection,” explains Dr. Cheung. “However, if the patient has an indwelling device, bacteria can home in on the device, preventing a thorough clearance of the infection unless the device is removed. For example, Staphylococcus aureus infections are known for their virulent course, the tendency to cause sepsis, and profound systemic symptoms. One of the hallmarks of the bacteria is that it can form a biofilm that serves as a protective mechanism which renders the pathogen resistant to intravenous antibiotics. This biofilm can form on the device, which enables the bacteria to hide and evade the usual antibiotic therapy. Unless the device is removed, antibiotics alone will not eradicate the infection.”
The research team looked at utilization of transvenous lead removal/extraction (TLE) among patients with CIEDs with infective endocarditis using the Nationwide Readmissions Database. The NRD contained 25,303 admission records between January 2016 and November 2019 that matched the study population criteria, including patients having a Class I indication for device system removal. Findings of their research, which were published in the May 2, 2023, issue of the Journal of the American College of Cardiology, revealed the following:
- Only 2,900 patients (11.5%) with CIEDs underwent TLE
- Overall rate of TLE-related complications was 2.7%
- Proportion of patients undergoing TLE management increased significantly from 7.6% in 2016 to 14.9%in 2019
- Index mortality was significantly lower among patients managed with TLE (6.0%versus 9.5%)
- Patients with S. aureus infections had significantly higher index mortality compared to patients without S. aureus infections (13.8%versus 7.8%)
- Presence of Staphylococcus aureus infection, implantable cardioverter-defibrillator, and large hospital size were independently associated with TLE management
To our knowledge, this is the first study to shine a light on a national, real-world level answer to the question, ‘What is the actual percentage of patients with cardiac devices and endocarditis who are being managed with lead extraction?’
— Dr. Jim Cheung
“When you seek to improve quality of care and when you want ensure that there is adherence to practice guidelines, the first step is to identify the scope of the problem,” says Dr. Cheung. “While the indications for device removal in patients with cardiac devices who develop an infection are well-known, we wanted to shine a light on a national, real-world level answer to the question, ‘What is the actual percentage of patients with cardiac devices and endocarditis who are being managed with lead extraction??’ If the number had been 70 or 80%, then that would be acceptable. However, when we found only a 12% rate of lead extraction use, we discovered that the scope of the problem is much greater than we had anticipated.”
Whys and Wherefores of Underutilization
Dr. Cheung explains that the underutilization of lead extraction and device removal are multifactorial.
Misleading Blood Cultures
One issue is a knowledge gap among physicians of the need to remove the entire system to completely clear an infection.
“In scenarios where a patient with a cardiac device presents with bacteremia or endocarditis is administered intravenous antibiotics and subsequently has multiple negative blood cultures, there can be a misconception that the bacteria has been completely eradicated,” says Dr. Cheung. “In addition, there can be a misconception that the skin pocket site of the device needs to red or painful for there to be an infection. When a survey conducted a few years ago with internal medicine doctors asked, ‘If a patient arrives with a staph aureus bacteremia with no evidence of device pocket involvement, do you just treat it with antibiotics or treat with device removal?’, only a minority of internal medicine physicians were aware of the indication to completely remove the device system.”
Indefinite Signs of Infection
Another misconception in recognizing CIED-associated infections is that a device can be infected without any signs seen on physician exam or imaging. “This misconception is based in the belief that you need to see vegetation on the lead with a transesophageal echocardiogram to identify that the device is involved in the infection,” says Dr. Cheung. “However, even if the transesophageal echocardiogram shows no evidence of vegetation, if the patient presents with refractory bacteremia or even high-grade bacteremia, the device and the leads still need to be taken out.”
Uncertainty about Procedural Risks
It is also important to understand the perception of the risks associated with lead extractions can pose a barrier to appropriate treatment. “What our study shows is that the actual risk of complications associated with lead extraction is quite low at less than 3%, says Dr. Cheung. “The likelihood of experiencing a mortality in the setting of having a lead extraction-associated complication was 0.4%. This is consistent with data from large registries compiled in Europe and in the United States which show that the risk of mortality associated with lead extractions, particularly when performed in experienced centers, is less than 1%.
Yet it is understandable why cardiologists and others are concerned about the risk of lead extractions. These can be high risk procedures, often involving the use of laser energy or other mechanical tools to remove leads, particularly when the leads have been in place for a long time which can lead to extensive fibrosis. However, when the procedure is performed in the appropriate setting, with a multidisciplinary team, cardiothoracic surgery backup, and availability of specialized tools, many major complications, such as superior vena cava tears, cardiac perforation, and tamponade can be managed expeditiously and safely.”
Optimizing Outcomes
Dr. Cheung emphasizes that at NewYork-Presbyterian/Weill Cornell Medicine, where the Cardiac Device Clinic cares for over 5,500 patients, a multidisciplinary approach involving general cardiologists, the electrophysiology service, infectious disease specialists, and cardiothoracic colleagues is key to caring for patients with CIED-associated infections. “Patients with cardiac devices often have very complicated medical histories, including cardiac and non-cardiac comorbidities that need to be addressed. So, it does take a team effort to make sure patients are optimized for the best possible outcome,” says Dr. Cheung. “When a patient presents with endocarditis and has a cardiac device, the general cardiology and electrophysiology teams are notified, and the patient is assessed and quickly scheduled for lead extraction and system removal if appropriate. Our procedures are performed in state-of-the-art hybrid operating rooms equipped with fluoroscopy and the capability to perform sternotomy and place patients on bypass. We collaborate with our cardiothoracic surgical team who provide important support in the very rare cases where they are needed.”
Dr. Cheung and his colleagues are also exploring digital electronic solutions to help improve the efficiency of their team-based approach. “Studies show that outcomes are better when the extraction or device removal occurs sooner in the patient's course. Our goal is to leverage the use of our electronic health records to flag patients with a diagnosis of endocarditis and septicemia, and to automate alerts to our team for those patients who have any history of an indwelling device so that we can initiate the appropriate consults without delay,” says Dr. Cheung.
“When our paper came out, the word on the street was that physicians were shocked at how so few patients were undergoing the recommended treatment of lead extraction and complete device removal to treat their CIED-associated infection,” notes Dr. Cheung. “Now that we have identified the scope of the problem, we can better prioritize areas to address, including the need to increase patient access to centers that have the experience, resources, and safeguards in place to ensure the best outcomes. We need to increase both patient and physician awareness of appropriate management of device-related infections. Education efforts should involve not just electrophysiologists and cardiologists, but also physicians of all specialties. Most patients presenting with an infection will first go see their primary care doctor or another specialist who has been caring for them – especially as the infection may not occur until months or years following their CIED implantation. By engaging those physicians as well, I think we can really move the needle towards increasing delivering the best care for patients with CIED infections and saving lives.”