A multidisciplinary team of psychiatry, neurology, cardiology, and general internal medicine clinicians across NewYork-Presbyterian/Columbia and the New York State Psychiatric Institute (NYSPI) recently conducted the first pilot of a novel treatment incorporating acceptance and mindfulness-based exposure therapy for PTSD after sudden cardiac arrest. The results were published in the Journal of Clinical Psychiatry.
Sudden cardiac arrest (SCA) is the third leading cause of death and kills one person every two minutes in the US alone. Of half a million Americans experiencing it every year, an estimated 60,000 SCA patients survive hospital discharge and need evidence-based treatments that foster an understanding to reduce some of the uncertainty and fear of the unknown. According to Sachin Agarwal, MD, MPH, a Neurocritical specialist at NewYork-Presbyterian/Columbia and director of the nation's first interdisciplinary, multispecialty NeuroCardiac Comprehensive Care Clinical & Research Program (N4C) at Columbia, SCA survivors have no memory of their event. “When they go into cardiac arrest, they go into a coma right away and they don’t have the memories of things before the event or part of the ICU stay,” he says. “After that, they start making new memories. So a lot of people do not have flashbacks or re-experiencing phenomena that are typically described in PTSD among war veterans.”
PTSD experienced by SCA survivors can present in many distinct ways, including hypervigilance around bodily symptoms, fear of future events, and lack of trust in one’s body. Despite experiencing an incredibly traumatic event, there are no SCA-specific psychiatric treatment protocols to effectively address these unique concerns.
A multidisciplinary approach to address mental health needs of cardiovascular event survivors
Early in his career, Dr. Agarwal developed an interest in the connection between neurology and cardiology. “It all started a decade ago when I had a patient who had a cardiac arrest and then she did not survive it, but the reason for her to go into cardiac arrest was that she had undiagnosed epilepsy which was misdiagnosed as panic attacks,” he says. “Her unfavorable outcome was also because her brain was injured beyond repair and that got me interested in cardiac arrest and the role of neurology in improving outcomes.”
When she was 36, Maja Bergman, Ph.D., a psychologist with Columbia Psychiatry and the NYSPI, experienced a sudden cardiac arrest out of the blue. She survived the harrowing event, and her experience led her to develop an interest in figuring out the best ways to help these survivors process their trauma and adapt to their new normal.
Dr. Agarwal heard about Dr. Bergman’s work from her mentor Yuval Neria, Ph.D., Director of the NewYork-Presbyterian Military Family Wellness Center and the Columbia University PTSD Research and Treatment Team, and it immediately piqued his interest. “When I heard about Maja and her experience and her willingness to create something that was tailored to cardiac arrest survivors, I thought it was a no-brainer,” says Dr. Agarwal.
Ian Kronish, MD, MPH, a general internist, Associate Director of the Center for Behavioral Cardiovascular Health, and Co-Director of the Hypertension Center at NewYork-Presbyterian/Columbia, also had deep interest in psychological distress and behaviors following cardiac events. Working with Donald Edmondson, PhD, MPH, the Director of the Center for Behavioral Cardiovascular Health, Dr. Kronish has been studying patients who have experienced acute cardiovascular events for years. “Initially I was focused more on acute coronary syndromes, like heart attacks,” says Dr. Kronish. “Later we connected with Dr. Agarwal and collaborated with him looking at cardiac arrest. We’ve been observing people and studying what happens to them in terms of their psychological distress and health behaviors. We were seeing this pattern of PTSD that was going underrecognized and untreated. Dr. Neria and Dr. Edmondson were already collaborating. This created a web of connections that made this research possible.”
Dr. Kronish also serves as Director of the National Institute of Aging-funded Roybal Center for Fearless Behavior Change at Columbia, and through this center, he aims to develop interventions that improve mental health, adherence to recommended health behaviors, and cardiovascular outcomes in patients who have experienced acute cardiovascular events. “Our center allows us to invest in investigators that wanted to do clinical trials testing interventions to reduce psychological distress after acute medical events,” says Dr. Kronish. “Through a network of people we've met over the years, [Dr. Agarwal, Dr. Bergman, and I] all connected.”
Drs. Kronish, Neria, and Bergman used funding from the Roybal Center, and collaborated with Dr. Agarwal for recruitment to conduct a pilot study looking at the feasibility and preliminary efficacy of acceptance and mindfulness-based exposure therapy (AMBET), a novel SCA-specific psychotherapy protocol developed by Dr. Bergman and Dr. Neria, in SCA survivors.
Addressing PTSD to decrease the risk of future cardiac events
The reason Drs. Kronish, Agarwal, and Bergman wanted to address PTSD in SCA survivors is because psychological stress and poor health behaviors are associated with increased risk of future cardiovascular events. “After cardiovascular events, patients become avoidant of certain health behaviors that remind them of their vulnerability,” says Dr. Kronish. “Internal bodily sensations that get heightened with physical activity can lead to avoidance of physical activity. We have strong data that shows more sedentary behavior, less physical activity, and lower adherence to day-to-day cardiovascular medications in patients with PTSD symptoms related to cardiovascular events. These poor health behaviors all increase risk of future events.”
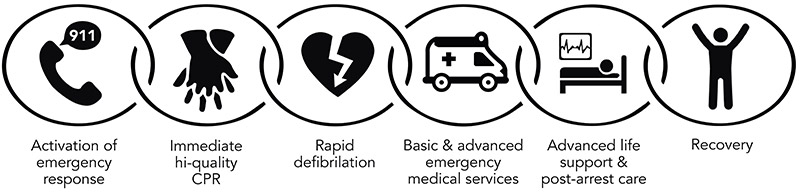
Universal adoption of the “sixth link” as part of the chain of survival to emphasize survivorship and recovery after cardiac arrest.
With that in mind. Drs. Kronish, Neria, Agarwal, and Bergman wanted to develop a protocol that would address both the trauma experienced by patients as well as the avoidance behaviors that place them at greater risk of future events. Dr. Bergman worked with Dr. Neria to combine different evidence-based interventions into a unique protocol specifically designed for SCA survivors. The study team hypothesized that AMBET would be feasible to deliver, well-liked by patients, and would have benefits two-fold:
- Reduction in PTSD symptoms, including hypervigilance to internal bodily stimuli
- Improvement in cardiovascular health behaviors post-SCA
The AMBET protocol involves gradual exposures, mindfulness, and cardiac psychoeducation. The exposures that are used include in vivo, interoceptive and imaginal and unique to each individual. “There may be really traumatic memories from their hospital stay, so they can create a narrative and walk through that,” says Dr. Bergman. “[The exposures] can be things like mild physical activity, being able to tolerate listening to your heart, and doing more mindfulness practices while observing different sensations in your body.”
Pilot study yields positive results
The study enrolled a small sample – 11 SCA survivors – who met the DSM-V PTSD criteria. “A lot of the patients had these [PTSD] symptoms for years,” says Dr. Kronish. “I think the shortest was 10 months post-cardiac arrest, but several were years afterward and several had tried other treatments and did not respond to them. This was not an easy group of people to treat.”
The participants engaged in eight 90-minute remotely delivered individual sessions and were assigned homework to do outside of sessions, including daily mindfulness and exposure practices. PTSD symptoms were assessed using the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) at baseline, midpoint, posttreatment, and three-month follow-up. In addition to measuring psychological response, participants were provided a wrist-worn Fitbit HR Inspire to continuously measure physical activity and sleep.
Of the 11 patients enrolled, 10 (91%) completed treatment, and satisfaction was high with no adverse events reported. At posttreatment, 80% showed significant treatment response and 70% achieved PTSD diagnostic remission. “Patients responded extremely well to AMBET,” says Dr. Bergman. “This is really something that I think was very healing for these patients. Their symptoms got a lot better for almost all our patients.”
The benefits were not just psychological but also physical. Daily average steps significantly increased with large effect sizes on paired samples t-test, from 7,110 (SD=5,378) to 9,297 (SD=5,600) (t=3.12, P=.026, g=-1.2). The baseline mean sleep duration remained in the normal range.
“This is a very inspiring study because there's not much out there about what works for these patients,” says Dr. Agarwal. “These patients really live with this feeling and condition for years and years and years. So this is very exciting for us and for the clinicians who are taking care of these patients.”
Looking toward the future
Drs. Agarwal, Kronish, and Bergman hope to conduct larger future studies to further validate the AMBET protocol among SCA survivors with PTSD. “In terms of next steps, we’re really looking at expanding this, doing it in a statistically powered randomized controlled trial, and possibly also expanding it beyond cardiac arrest to other kinds of acute cardiac events,” says Dr. Bergman.
Dr. Agarwal shares similar sentiments. “I feel the future direction of this work is that it should be given or offered early and then see if you can even prevent these symptoms from becoming a disorder,” he says. “So I see early interventions as a future direction, and I see combining it with other interventions that are coming out of the Roybal Center and seeing if the combinations are better than the individual therapies.”
Incorporating the family into the treatment is also an avenue of interest. “There’s a lot of focus now on interventions that include the families because there are a lot of families who witness [the sudden cardiac arrest], participate in the resuscitation, and initial CPR. They have their own trauma that has not been addressed by anyone because no one thinks of family members that way,” says Dr. Agarwal.
Dr. Kronish says there’s a lot that can be learned from this study. “This study highlights the importance of integrating behavioral and psychiatric care into the management of cardiovascular disease, which we know historically our health system has not been particularly good at,” he says. “The more that we can develop these integrated programs, like Dr. Agarwal’s developing with his cardiac survivors program of research and clinical care, that’s what I’m hoping to inspire through our Roybal Center and my own research and personal interests.”
NewYork-Presbyterian/Columbia provides the right landscape to conduct this type of trial with its focus on cardiac arrest survivorship. “If I look at the number of departments, divisions, and specialties that are involved in our NeuroCardiac program and the Roybal Center, you're going to see almost everyone because it's the whole body that gets hurt after cardiac arrest,” says Dr. Agarwal. “It’s a perfect setting to understand life-threatening emergencies and community-based emergencies. It’s going to take a village to make a small dent into survival and then survivorship. Columbia is the central clearing house for all the survivorship work that goes on nationally and then picked up internationally. If this kind of work has legs, I think it should be tested here first.”




