Current Thinking on Bone Health

Dr. Linda A. Russell
Osteoporosis has long been called a silent disease since there are no warning signs or symptoms until fractures occur. In the United States alone, an estimated 1.5 million fractures each year are attributed to low bone density. “And the risks of osteoporosis are not relegated exclusively to women — males represent 20 percent of all cases,” says rheumatologist Linda A. Russell, MD, Director of the Osteoporosis and Metabolic Bone Health Center at Hospital for Special Surgery. For more than 30 years, the Center — which was the first program of its kind in the nation — has pursued its mission to prevent osteoporosis and to provide treatment options that promote bone health. Today, the Center is the only one in New York City that that holds the International Society for Clinical Densitometry Facility Accreditation.
In addition to evaluating and caring for patients with metabolic bone disease, Dr. Russell, who is also Director of Perioperative Medicine at Hospital for Special Surgery, has focused her attention on perioperative bone health, leading a team that includes specialists in rheumatology, endocrinology, and orthopedics. “We evaluate the bone health of a range of patients beyond those individuals whose age puts them at risk for osteopenia or osteoporosis,” says Dr. Russell. “These include patients taking medications that cause bone loss, such as glucocorticoids to treat chronic obstructive pulmonary disease, asthma, colitis, and rheumatoid arthritis, and aromatase inhibitors that are used to treat breast cancer. These two, in particular, are very common medications that contribute to bone loss and would warrant a patient’s evaluation for metabolic bone health. In addition, certain conditions, such as celiac disease and multiple myeloma, predispose someone to bone loss, so we also screen for those when individuals present with osteoporosis or fracture.”
Dr. Russell and her colleagues will also evaluate adults who have suffered low-impact fractures and those who are preparing to have major orthopedic procedures, such as a spine fusion or a revision total hip replacement. “We will test these patients preoperatively and, if indicated, put them on a treatment plan so that their bone is as strong as possible for surgery,” she says.
Measuring Bone Loss Today
In addition to the standard bone densitometry test (DEXA) to measure bone loss, Center physicians also obtain a trabecular bone score (TBS), which indicates the porosity of a vertebral body as a measure of the strength and quality of the bone. “TBS is related to bone microarchitecture and provides skeletal information that is not captured by the standard bone mineral density measurement,” says Dr. Russell. “In a current study, we are also using TBS for patients with ankylosing spondylitis because of its possible greater accuracy as a fracture risk assessment tool.”
At the time the DEXA is obtained, a patient can also have a femur fracture assessment. This test gives a pictoral view of both femurs. Cortical thickness can be assessed; when increased, it may be a sign of an impending atypical femur fracture.
FRAX® is a fracture risk assessment tool that can evaluate the 10-year probability of a person’s risk of fracture. This tool can be used to determine if a patient is at high risk for fracture when the DEXA scan indicates low bone mass. FRAX is based on risk factors such as age, weight, family or personal history of fracture, glucocorticoid use, diagnosis of rheumatoid arthritis, as well as bone density of the femoral neck. According to World Health Organization guidelines, treatment is recommended if the FRAX analysis shows a risk of any fragility fracture >20 percent in 10 years or a risk of hip fracture >3 percent.
Making Sense of Medications
Initially, the mainstay of treatment for osteoporosis was hormone replacement therapy, followed by bisphosphonates, which over the last few years has been the subject of controversy. “The first class of medications that we were using for the treatment of osteoporosis was the bisphosphonates,” explains Dr. Russell. “We learned that if you take these medications for a prolonged period of time, more than 5 or 10 years without a holiday, there is an increased risk of osteonecrosis of the jaw and atypical femoral fracture. Though these are unusual and rare occurrences, many patients worry about them tremendously. Then about five years ago, an article came out saying the bisphosphonates were harmful and then everyone stopped taking them.”
When the number of hip fractures started to increase again, notes Dr. Russell, the medical world reconsidered their use. “Our current thinking is that we do want to use these medications when people are at high risk for fracture,” says Dr. Russell. “But now, after patients have been on them for a while, we give periodic holidays from this therapy.”
Denosumab, a human anti-RANK ligand antibody, has shown to induce sustained inhibition of bone resorption lasting for months after a single subcutaneous injection. “Denosumab is also an antiresorptive agent,” says Dr. Russell. “Denosumab is FDA approved for the treatment of osteoporosis in postmenopausal women at high risk of fracture, male osteoporosis, and for patients with cancer-induced bone loss. Teriparatide and abaloparatide are both anabolic agents; these agents promote bone formation. They can help reduce the risk of fractures and can aid in fracture healing.”
Dr. Russell emphasizes that adults who have had a low impact fracture are at great risk for another fracture if left untreated and should be referred for testing and evaluation. “At our Center, patients are tested and then their case is presented to an interdisciplinary team,” she says. “The final recommendations are given to the patient and their primary care physician.”
Contributing Factors to Atypical Femoral Fracture
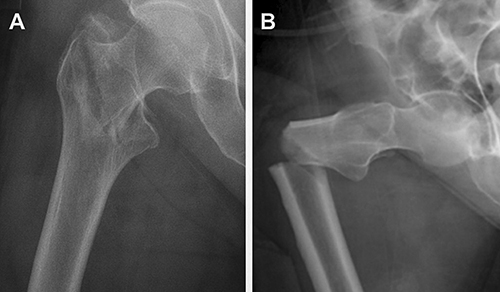
Radiograph imaging showing morphology of a typical fragility fracture of the hip (A), compared with an atypical femoral fracture, or AFF (B). The nature of the AFF indicates a brittle fracture process, possibly due to excess mineralization of the bone. (Courtesy of Donnelly Research Lab)
A study conducted by faculty in the Department of Materials Science and Engineering at Cornell University in collaboration with researchers from Hospital for Special Surgery and Weill Cornell Medicine has shed light on why prolonged use of bisphosphonates can alter the composition of bone, making it more brittle and susceptible to atypical femoral fracture (AFF). The researchers examined biopsies of cortical bone from the shaft of the femur obtained from postmenopausal women during fracture repair surgery. The participants were placed in five groups, based on fracture type and bisphosphonate use.
Their findings indicated that the bone of women treated with bisphosphonates who had AFF was harder and more mineralized than bisphosphonate-treated women with typical osteoporotic fractures. The main function of bisphosphonates is to slow down the resorption of old bone, which is generally followed by remodeling. In healthy adults, cortical bone is constantly being resurfaced, but if that resurfacing process begins with resorption, and if resorption is slowed by bisphosphonates, the remodeling process is also affected. The result is that existing bone ages and becomes brittle over time.
Long-term bisphosphonate use also involves crack-deflection — the ability of the resurfaced bone to stop a microscopic crack from propagating, which can lead to a break. New layers of bone can act as a “firewall” of sorts, stopping a crack from spreading, but mineralized, older bone loses that function.
The FDA is now recommending patients use bisphosphonates for three to five years, followed by reassessment of their risk. “What we have observed is really the result of long-term treatment, well beyond what the FDA is recommending for these drugs now,” says Eve Donnelly, PhD, Assistant Professor in the Department of Materials Science and Engineering at Cornell University. “Our work explains some of the underlying mechanisms of AFFs and can inform the refinement of dosing schedules for patients at risk of fragility fractures.”
Reference Article
Lloyd AA, Gludovatz B, Riedel C, Luengo EA, Saiyed R, Marty E, Lorich DG, Lane JM, Ritchie RO, Busse B, Donnelly E. Atypical fracture with long-term bisphosphonate therapy is associated with altered cortical composition and reduced fracture resistance. Proceedings of the National Academy of Sciences USA. 2017 Aug 15;114(33):8722-27.
Related Publications





