Columbia Orthopedics: Leading the Field in Sports Medicine
In This Article:
Our Team Physicians: Overseeing Player Health
Professional
- The New York Yankees
Dr. Christopher S. Ahmad
Head Team Physician - New York City Football Club
Dr. Christopher S. Ahmad
Head Team Physician - USA Hockey
Dr. Charles A. Popkin
Team Physician - Jersey Hitmen Ice Hockey
Dr. Thomas S. Bottiglieri
Head Team Physician - The Armory Foundation
Head Team Physicians
Collegiate
- Columbia University
Dr. William N. Levine
Head Team Physician - Dr. Natasha Desai
Associate Team Physician - Fordham University
Dr. Elan Goldwaser
Head Team Physician - Dr. Charles A. Popkin
Head Team Orthopedist - Manhattan College
Dr. David P. Trofa
Head Team Physician - Mercy College
Dr. Charles A. Popkin
Head Team Physician - Dr. Elan Goldwaser
Associate Team Physician - Nyack College
Dr. Thomas S. Bottiglieri
Head Team Physician - Pace University
Dr. Nicole S. Belkin
Head Team Physician
Treating athletes at all levels of performance requires an in-depth knowledge and understanding of the demands placed on the musculoskeletal system by the rigors of training and competition in all variety of sports. It also requires precise skills and training in caring for high-performing competitors, where expeditious treatment and recovery are critical to staying in the game.
This highly specialized expertise is found in the Center for Shoulder, Elbow and Sports Medicine in the Department of Orthopedic Surgery at NewYork-Presbyterian/Columbia University Irving Medical Center. Our sports medicine physicians, many of whom have been competitive athletes, have a distinguished record of returning players to their sport in optimal form.
Under the leadership of Christopher S. Ahmad, MD, Chief of Sports Medicine and Vice Chair of Clinical Research for Columbia Orthopedics, the Center’s faculty of 13 orthopedic surgeons and sports medicine physicians is dedicated to treating athletic injuries of the musculoskeletal system. In the following article, Dr. Ahmad, Charles A. Popkin, MD, and David P. Trofa, MD, provide an update on clinical initiatives and research activities in their respective areas of expertise.
Spearheading the Management of Tommy John Injuries
“My life’s work and mission has been on how to improve Tommy John surgery, prevent Tommy John surgery, and study it in every capacity at every level of athletic performance,” says Dr. Christopher Ahmad, Head Team Physician for the New York Yankees and the New York Football Club and a member of the Advisory Committee of the Major League Baseball Team Physicians Association.
Dr. Christopher S. Ahmad
According to Dr. Ahmad, Tommy John surgeries are becoming widespread, if not routine, in the major leagues and indeed are on the rise. “Velocity is the most direct link to the force on the ulnar collateral ligament, and every year the average fast ball velocity is increasing in major league baseball leading to more UCL injuries and Tommy John surgeries,” says Dr. Ahmad, who has researched this topic extensively. “In one study, we looked at pitchers who had thrown complete games and compared them to a control group – pitchers on a major league level who did not throw a complete game – and we found something astonishing. If a pitcher throws a complete game, the chance of going on the disabled list is 74 percent. A control group of players never having thrown a complete game go on the disabled list at a rate of 20 percent.”
Dr. Ahmad is also concerned over the prevalence of UCL surgery among youth athletes, who are throwing with more velocity and more volume. “It is now obvious that youth athletes are at a disturbing risk for throwing-related injuries,” says Dr. Ahmad, who notes that the 17- to 18- year-olds are needing UCL surgery the most. “In fact, major league baseball clubs are consistently drafting young players who have already had ulnar collateral ligament reconstruction.”
With the support of Major League Baseball, Dr. Ahmad established The Pitch Registry in May 2019 to better understand pitching injuries and how they can be prevented and to serve as a platform for research and education. “This registry enables us to enroll several thousand individuals needing Tommy John surgery,” he says. “We enter the necessary preoperative and intraoperative data into the registry, such as the patients’ MRI features and what happens during the surgery. The registry has been formulated with a dynamic platform and a user interface so that our patients can enter online important data pertaining to their rehabilitation. Then if a patient comes in a year from now and says, ‘I have a loose chip in my elbow, and I’m a lefty, and I have a partial tear, what’s the best treatment?’ Before we didn’t have the perfect answer, whether it’s arthroscopy in combination with the Tommy John surgery versus arthroscopy plus a repair or just a repair surgery. This data will give us answers that we can then use to guide treatment approaches for players, as well as educate parents and coaches.”
Dr. Ahmad also participated in the development of a comprehensive multicenter report on current trends, surgical techniques, and outcomes of revision UCL reconstructions performed on professional baseball pitchers between 2010 and 2016. The study showed return to play rates following revision UCL reconstruction at 77 percent, however, only 55 percent of players returned to their same level of play.
Read more:
Camp CL, Desai V, Conte S, Ahmad CS, Ciccotti M, Dines JS, Altchek DW, D'Angelo J, Griffith TB. Revision ulnar collateral ligament reconstruction in professional baseball: Current trends, surgical techniques, and outcomes. Orthopaedic Journal of Sports Medicine. 2019 Aug 14;7(8):2325967119864104.
Classifying Partial Patellar Tendon Tears
In a study on patellar tendinopathy, which frequently affects athletes involved in jumping sports, Dr. Popkin and the Columbia sports medicine team sought to define the relationship between partial patellar tendon tear (PPTT) characteristics and treatment guidelines, as well as develop an MRI-based classification system for these injuries. Current classifications of patellar tendinopathy are based on symptoms and do not provide satisfactory evidence-based treatment guidelines.
The researchers noted that partial-thickness tears are located posterior or posteromedially in the proximal patellar tendon. The most sensitive predictor for detecting the presence of a partial tear was patellar tendon thickness and tracking thickness changes on axial MRI may predict the effectiveness of nonoperative therapy. Based on their results, the authors developed the Popkin-Golman classification, a novel classification system proposed for partial tears that can be used to guide treatment decisions for these patients. “We believe this study is changing the way people are treating and thinking about that injury,” says Dr. Popkin.
Read more:
Golman M, Wright ML, Wong TT, Lynch TS, Ahmad CS, Thomopoulos S, Popkin CA. Rethinking patellar tendinopathy and partial patellar tendon tears: A novel classification system. American Journal of Sports Medicine. 2020 Feb;48(2):359-69.
Pursuing Novel Techniques for ACL Reconstruction
David P. Trofa, MD, specializes in the operative and non-operative treatment of athletes of all ages and skill levels with expertise in arthroscopic and open surgery of the knee and shoulder. “My subspecialty practice is primarily focused on complex knee pathology, including meniscus, ligamentous, and articular cartilage pathology,” says Dr. Trofa.
Dr. Trofa’s clinical and basic science research endeavors also include methods of improving the latest cartilage restoration and preservation techniques, leveraging orthobiologic therapies to provide athletes with a full spectrum of treatment options, and improving outcomes associated with anterior cruciate ligament (ACL) reconstructions.
Dr. David P. Trofa
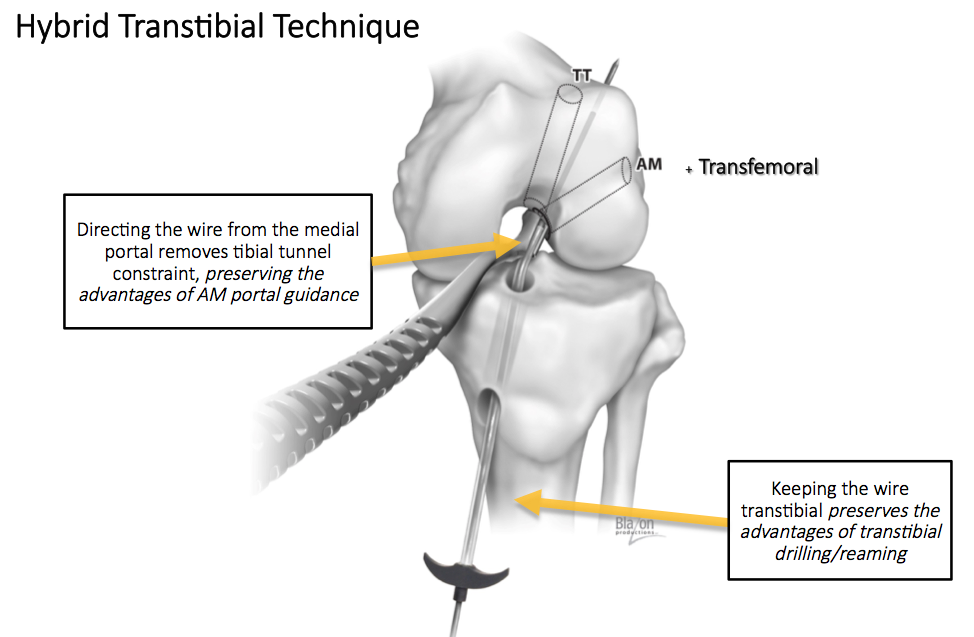
Research has shown the importance of anatomic graft placement during ACL reconstruction to optimize both biomechanical and clinical outcomes. Dr. Trofa was the first author on a randomized controlled trial performed in collaboration with Dr. Dana Piasecki of OrthoCarolina, who developed a hybrid transtibial technique using medial portal guidance of a flexible transtibial guidewire that incorporates the strengths of both the anteromedial portal and the transtibial approaches.
The researchers found that by maintaining a transtibial trajectory for femoral tunnel reaming, the hybrid approach preserved the beneficial features of a traditional transtibial technique, including the avoidance of knee hyperflexion, elimination of the risk of iatrogenic injury to the medial femoral condyle, and favorable femoral tunnel characteristics. Further, guidance of the transtibial guidewire through the anteromedial portal removed any tibial tunnel constraint allowing for anatomic aperture positioning of the femoral tunnel.
Courtesy of DanaMed
“We believe that this approach has all the advantages of tibial independent femoral tunnel drilling techniques, while not sacrificing the benefits of the more traditional transtibial technique,” says Dr. Trofa. “The hybrid transtibial approach with the Pathfinder™ guide (DanaMed, Inc.) allows for anatomic ACL positioning without compromising the trajectory of the tunnel.”
In the study, the results of which were published in the November 2020 issue of the American Journal of Sports Medicine, 30 consecutive patients with primary ACL tears were randomized to undergo the transtibial, anteromedial portal, or hybrid transtibial technique for femoral tunnel drilling at the time of reconstruction. All patients underwent 3-dimensional computed tomography of the knee at six weeks postoperatively and measurements were taken of femoral and tibial tunnel aperture positions and tunnel lengths. The research team concluded that the hybrid technique achieved femoral aperture positions equally as anatomic as the anteromedial portal technique, but produced longer, less angulated femoral tunnels, which may help reduce graft strain and mismatch.
In other ACL reconstruction research, Dr. Trofa and his Columbia colleagues are evaluating patient preferences for various graft types (including hamstring, bone-patellar tendon-bone, and quadriceps tendon), fixation methods, and internal bracing as a means of accelerating postoperative rehabilitation and return to play.
Read more:
Trofa DP, Saltzman BM, Corpus KT, Connor PM, Fleischli JE, Piasecki DP. A Hybrid Transtibial Technique Combines the Advantages of Anteromedial Portal and Transtibial Approaches: A Prospective Randomized Controlled Trial. American Journal of Sports Medicine. 2020 Nov;48(13):3200-3207.
Promoting Safety on the Ice
With dual fellowships in Sports Medicine and Pediatric Orthopedics, Dr. Charles A. Popkin has dedicated his career to the comprehensive treatment and prevention of injury in developing athletes. He has a particular interest in the management of ice hockey injuries, serving as a team physician for USA Hockey, and on the USA Hockey National Safety and Protective Equipment Committee. Dr. Popkin is also the head team physician for the Mercy College Mavericks in Dobbs Ferry, and the Hackley School in Tarrytown.
Dr. Charles A. Popkin with Seth Appert, former Head Coach of USA Hockey’s National Team Development Program and now Head Coach of the Rochester Americans.
“I grew up in Minnesota, where I played hockey and then played football in college. But hockey was always my true love,” says Dr. Popkin, who served as the Head Team Physician for the National Men’s Hockey Team in 2018, and subsequently was appointed to the Safety and Protective Equipment Committee of USA Hockey. “Whereas the incidence of football injuries has been dropping, the number of hockey injuries has increased. What is rewarding to me about being on the Safety and Protective Equipment Committee is that we have the opportunity to try to make a game that I’m passionate about as safe as possible to play.”
Among Dr. Popkin’s research initiatives is a focus on the epidemiology of foot and ankle injuries in collegiate ice hockey. In an article published in the Orthopaedic Journal of Sports Medicine in August 2019, Dr. Popkin and colleagues reported on a multicenter study that showed foot and ankle injuries were frequent among collegiate ice hockey players. The investigators noted: “For men, contusions were the most commonly diagnosed injury, although high ankle sprains resulted in the most significant time lost. For women, low ankle sprains were the most common and resulted in the most moderate time lost. These findings may direct future injury prevention and guide improvements in ice skate design.”
“The incidence of foot and ankle injuries has been fairly overlooked in hockey. Previously the thinking had been that there were a lot of high ankle sprains because of the boot,” says Dr. Popkin. “We uncovered in this study that a fair number of hockey players still get lower ankle sprains, too.”
Body checking is a common cause of youth ice hockey injuries, and consequently, in 2011, USA Hockey raised the minimum age at which body checking is permitted from the Pee Wee level (11 to 12 years old) to the Bantam level (13 to 14 years old). Dr. Popkin participated in a study to determine the impact of body checking on the distribution of injuries reported in youth ice hockey players, hypothesizing that the elimination of body checking at the Pee Wee level would lower the frequency of serious injuries, particularly concussions.
“Using the National Electronic Injury Surveillance System, we looked at the number of kids nationally that presented to the ER both before and after USA Hockey changed the rule,” says Dr. Popkin. “We found that overall injuries decreased by 16 percent in Pee Wee players, with injuries caused by body checking decreasing by 40 percent. Interestingly, the number of concussions in the younger group, despite the checking changes, actually went up. We thought that was because of a reporting bias, that concussion was now more on everybody’s radar and not because checking was not allowed.” Results of this study were published in the December 2017 issue of the Orthopaedic Journal of Sports Medicine.
“Women’s hockey is actually the greatest offender for concussion,” adds Dr. Popkin. “Even though there is not supposed to be checking, there is still a tremendous amount of collision. Research has shown that the female brain is also a little more susceptible to concussion. At safety summits, they’ve now made it a major penalty to check somebody from behind, which poses risk both for concussion and a cervical spine injury. Hits to the head are now illegal and also incur a major penalty. There is more awareness that repetitive hits to the head do take a toll over time.”
Going forward, Dr. Popkin envisions the implementation of forearm and ankle Kevlar for body protection to minimize skate lacerations. “Some of the recent data has shown that neck guards are a good idea, too,” he says. “Hopefully we can develop something skaters can wear underneath that is all Kevlar that would minimize the slashing and skate injury component, but still be breathable and not cumbersome to wear. Shoulder pads should also undergo modifications as there is a hidden epidemic of clavicle fractures in ice hockey and that is something I am in the initial phases of studying.”
Read more:
Crowley SG, Trofa DP, Vosseller JT, Gorroochurn P, Redler LH, Schiu B, Popkin CA. Epidemiology of foot and ankle injuries in national collegiate athletic association men’s and women’s ice hockey. Orthopaedic Journal of Sports Medicine. 2019 Aug 28;7(8):2325967119865908.
Trofa DP, Park CN, Noticewala MS, Lynch TS, Ahmad CS, Popkin CA. The impact of body checking on youth ice hockey injuries. Orthopaedic Journal of Sports Medicine. 2017 Dec 5;5(12):2325967117741647.
Investigating Injuries in the Athletic Youth
Risks of Overspecialization
“In studying aspects of sports specialization, a phenomenon that we call early professionalization, we found that coaches and parents are not aware of how devastating overspecialization can be,” says Dr. Ahmad. “Also, we learned that the demands from coaches on their players are extreme. As an example, we surveyed kids in New Jersey and New York communities and found that more than 50 percent felt that at an early age their coaches pressured them to stop playing multiple sports because it would detract from their skill development within that sport. The coaches, of course, are big influences – a youngster can’t say no to a coach.”
In a study published in the July 2019 issue of Orthopaedic Journal of Sports Medicine, Dr. Ahmad and his colleagues looked at Major League Baseball players to determine which athletes played more than one sport besides baseball in high school and if that had a positive effect on their health as an adult professional player. “The ones that played multiple sports in high school, in fact, had less injury rate as a professional player,” says Dr. Ahmad. “We can now go to parents and coaches and say it’s better if young athletes play multiple sports, even in high school, so that they give their body a rest from the overuse of specific muscles. For example, if you’re a baseball player, your elbow is at risk for injury if you don’t have any time to rest. But if you play basketball in the winter, you get a rest period from it. So, for the first time, we can speak directly to the biggest influencers on young player health and those are parents and coaches.”
In a subsequent study published in the October 2020 issue of The Orthopedic Clinics of North America, Columbia orthopedic surgeons also supported the finding that early sports specialization “leads to increased risk of injury, higher rates of burnout, and lower lifelong sports participation without increasing elite achievement,” with throwing athletes particularly vulnerable to overuse injuries of the shoulder and elbow.
Read more:
Anderson FL, Knudsen ML, Ahmad CS, Popkin CA. Current trends and impact of early sports specialization in the throwing athlete. The Orthopedic Clinics of North America. 2020 Oct;51(4):517-525.
Confino J, Irvine JN, O’Connor M, Ahmad CS, Lynch TS. Early sports specialization is associated with upper extremity injuries in throwers and fewer games played in Major League Baseball. Orthopaedic Journal of Sports Medicine. 2019 Jul 26;7(7):2325967119861101.
Adolescent ACL Injuries
Tears and injuries of the anterior cruciate ligament are rampant in youth sports, with studies showing that the rate of ACL injuries is increasing as sports participation increases. Dr. Popkin and his Columbia colleagues published results of their survey – Trends in Management and Complications of Anterior Cruciate Ligament Injuries in Pediatric Patients: A Survey of the PRiSM Society – in the Journal of Pediatric Orthopaedics in 2018. The 15-question survey was distributed to 71 orthopedic members of the Pediatric Research in Sports Medicine (PRiSM) Society asking about their experience with the management and complications of ACL injuries.
“The most significant thing we learned is that surgeons were being a little more aggressive treating patients that had more than two years of growth remaining,” says Dr. Popkin. “Whenever you operate on an adolescent, the real risk is injury to the growth plate, which can cause either a leg length difference or an angular deformity. Our overall conclusion was the rate of growth disturbance is low, but we’re still identifying cases and so it needs to be part of the decision-making.”
Dr. Popkin and his colleagues also conducted several studies on ACL injuries, including looking at the wide range of rehabilitation protocols across the country. “Given the substantial variability observed among these protocols, our study suggests that standardizing pediatric ACL reconstruction rehabilitation has the potential to optimize patient care,” says Dr. Popkin. Results of this study appeared in the November 2019 issue of the Physician and Sportsmedicine.
Read more:
Forrester LA, Schweppe EA, Popkin CA. Variability in rehabilitation protocols following pediatric anterior cruciate ligament (ACL) reconstruction. The Physician and Sportsmedicine. 2019 Nov;47(4):448-54.
Popkin CA, Wright ML, Pennock AT, Vogel LA, Padaki A, Redler LH, Ahmad CS. Trends in management and complications of anterior cruciate ligament injuries in pediatric patients: A survey of the PRiSM Society. Journal of Pediatric Orthopaedics. 2018 Feb;38(2):e61-e65.
Engineering Osteochondral Replacement Tissue for Clinical Application
Dr. Trofa is currently collaborating with Clark T. Hung, PhD, Professor of Biomedical Engineering and Orthopedic Sciences (in Orthopedic Surgery) and Director of the Cellular Engineering Laboratory at Columbia, on a number of research grants aimed at strategies to optimize donor tissue for cartilage transplantation.
“Collaboration between basic scientists and clinicians is paramount to advance our treatment algorithms for cartilage pathology,” says Dr. Trofa. “Currently, our best treatment for a large symptomatic focal cartilage lesion is an osteochondral allograft transplantation, but the success often depends on the viability of the tissue. Dr. Hung and I are particularly interested in improving the viability of the implanted tissue to enhance the functional outcomes associated with allograft osteochondral transplantations.”
Dr. Hung and his laboratory previously developed a media, Missouri Osteochondral Allograft Preservation System (MOPS), which was found to preserve grafts twice as long as standard of care media. As a result of these and similar findings, MOPS is currently used by the Musculoskeletal Transplant Foundation (MTF) for graft storage. “Together, Dr. Hung and I are studying another media which we are hoping will further optimize donor tissue. We are also investigating surgical instrumentation that can be used during the procedure that might result in greater cell viability at the time of implantation,” says Dr. Trofa. “So much about this operation depends on the number of viable cells implanted at time zero.”
Read more:
Nover AB, Stefani RM, Lee SL, Ateshian GA, Stoker AM, Cook JL, Hung CT. Long-term storage and preservation of tissue engineered articular cartilage. Journal of Orthopaedic Research. 2016 Jan;34(1):141-8.