Establishing Practice Guidelines for Endoscopic Evaluation of Altered Bowel Anatomy
Patients with inflammatory bowel disease (IBD) frequently undergo surgical treatment that can result in considerable changes to their bowel anatomy, rendering subsequent diagnostic and therapeutic endoscopy challenging to perform. While practice guidelines from professional societies are available for the diagnosis and management of IBD, published guidelines related to the endoscopic interventions for patients following IBD surgery were not.
Dr. Bo Shen
With this in mind, Bo Shen, MD, Director of the Center for Interventional IBD at NewYork-Presbyterian/Columbia University Irving Medical Center, and Vice Chair for Innovation in Medicine and Surgery at Columbia, brought together experts in the field to form a worldwide consortium focused on establishing consensus guidelines for best practices related to interventional IBD. As a pioneer in IBD treatment incorporating endoscopic approaches and with over 30 years of experience in the field, Dr. Shen led the 31-member group of nationally and internationally renowned IBD specialists. Gastroenterologists, GI surgeons, advanced endoscopists, pathologists, and radiologists representing the United States, Canada, Europe, Asia, and South America participated in this prodigious undertaking.
“Our worldwide group of investigators – all experts in their own right – met via Zoom and, using the Delphi procedure, generated some 60-plus statements to consider,” says Dr. Shen. “Only those items receiving 80 percent approval were included in the final guideline. It was a complex process with vigorous discussions, multiple revisions, and two rounds of voting.”
At the conclusion of the process, the consortium produced a comprehensive consensus guideline that outlines anatomies frequently seen at endoscopy in the surgically altered bowel in healthy and diseased states and provides principles and techniques of endoscopy in these patients.
At a Glance
The practice guidelines, published in the June 2021 issue of The Lancet. Gastroenterology & Hepatology, focused on the eight procedures listed below. Each statement is associated with a level of evidence with a score of 1 to 5, with 1 indicating the strongest evidence, and a level of recommendation graded from A to D, with A signifying the highest recommendation. Following are a few abbreviated statements from the guidelines.
Preprocedural preparation
Cross-sectional imaging or small bowel series should be obtained before endoscopy in patients with suspected strictures, fistulas, or abscesses. (Evidence 2; Recommendation B)
Bowel resection and anastomosis
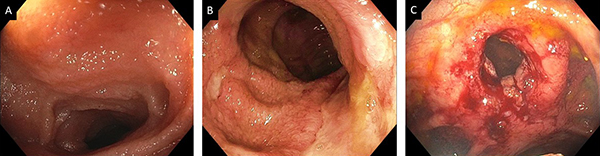
The first postoperative ileocolonoscopy should be done at 6 to 12 months post-ileocolonic resection for disease monitoring and possible delivery of endoscopic therapy. (Evidence 1; Recommendation A) Recurrent Crohn’s disease of the neo-terminal ileum is assessed by the Rutgeerts score.
Figure 1: Assessment of disease activity of Crohn’s disease after ileocolonic resection and anastomosis. A. Normal neoterminal ileum (I0); B. Large ulcers in the neo-terminal ileum (I4); C. Ileocolonic anastomotic stricture (I4) status post of balloon dilation.
Stoma
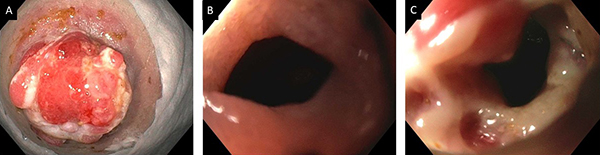
The endoscopist should carefully review and document the configuration of the ileostomy or colostomy before scoping via the stoma. (Evidence 4; Recommendation B) Intubation should be at least 10 cm beyond the stoma. Activity of Crohn’s disease can also be assessed by the Rutgeerts score.
Figure 2: Assessment of disease activity of Crohn’s disease in patients with ileostomy. A. Stomal stenosis; B. Extrinsic stenosis from the fascia pinch; C. Ulcerated stricture at the neo-terminal ileum (I4 lesions).
Ileal pouch
In patients suspected of having strictures, attention should be paid during pouchoscopy to areas prone to the formation of strictures, i.e., the stoma site, inlet, and pouch-anal anastomosis. Differential diagnoses of both ulcerated and non-ulcerated strictures in those areas include Crohn’s disease, surgical ischemia, or medication use. (Evidence 2; Recommendation A)
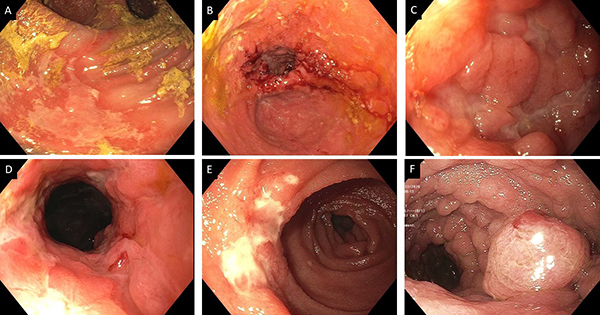
Figure 3: Inflammatory disorders of the pouch. A. C. difficile pouchitis with pseudomembrane; B. Ischemic pouchitis; C. Prepouch ileitis; D. Cuffitis; E. Crohn’s disease involving prepouch afferent limb; F. Inflammatory pseudopolyps.
Diverted bowel
Yearly surveillance endoscopy of the diverted large bowel is recommended for patients at risk of dysplasia. The location and number of biopsies depend on which anorectal or bowel segments were affected by IBD before faecal diversion. (Evidence 4; Recommendation C)
Strictureplasty
Capsule endoscopy is not recommended for the assessment of the activity of Crohn’s disease in patients with strictureplasty because of the risk of capsule retention. (Evidence 5; Recommendation C)
Bypass surgery
The bypassed duodenum, along with the stomach, proximal jejunostomy, and gastrojejunal or duodenojejunal anastomosis, should be closely monitored with upper gastrointestinal endoscopy for signs of Crohn’s disease. (Evidence 5; Recommendation D)
Immediate postoperative endoscopy
Immediate postoperative emergency endoscopy for the diagnosis and treatment of complications of IBD surgery can be done by an experienced endoscopist, with consideration of the risks and benefits. (Evidence 5; Recommendation D)
“Our document categorizes the different types of IBD surgery and addresses how to standardize the evaluation of postoperative anatomy,” says Dr. Shen. ”For example, how do you distinguish a surgery-related ulcer from Crohn’s disease? If it is surgery related, medication is not indicated. If it’s Crohn’s disease, medical management will be needed. We include endoscopic documentation, how to score or measure the disease, and how deep to insert your endoscope. Making the right call is critical and where the guideline for standards of practice can contribute.”
Center for Interventional IBD and Center for Ileal Pouch Disorders
Dr. Bo Shen
Dr. P. Ravi Kiran
The Center for Interventional IBD and Center for Ileal Pouch Disorders at NewYork-Presbyterian/
Read More
Endoscopic evaluation of surgically altered bowel in inflammatory bowel disease: a consensus guideline from the Global Interventional Inflammatory Bowel Disease Group. Shen B, Kochhar GS, Navaneethan U, Cross RK, Farraye FA, Iacucci M, Schwartz DA, Gonzalez-Lama Y, Schairer J, Kiran RP, Kotze PG, Kobayashi T, Bortlik M, Liu X, Levy AN, González Suárez B, Tang SJ, Coelho-Prabhu N, Lukas M, Bruining DH, El-Hachem S, Charles RJ, Chen Y, Sood A, Mao R, Loras C, Dulai PS, Picoraro JA, Chiorean M, Lukas M, Shergill A, Silverberg MS, Sandborn WJ, Bernstein CN. The Lancet. Gastroenterology & Hepatology. 2021 Jun;6(6):482-497.
Related Publications