Weill Cornell Medicine Sean Parker Institute for the Voice: Clinical Care Informed by Research
In September 2013, the Department of Otolaryngology – Head and Neck Surgery at Weill Cornell Medicine established the Sean Parker Institute for the Voice to offer expert diagnosis and advanced therapies covering the spectrum of voice disorders. Sean Parker Institute laryngologists at NewYork-Presbyterian/Weill Cornell Medical Center provide expertise in the medical and microsurgical treatment of injuries of the vocal fold from voice use, particularly in performers, and in neurologic voice disorders, including vocal fold paralysis and paresis, spasmodic dysphonia, and tremor.
The Institute has also developed a robust research program to support progress in understanding the origins and advancing treatment for some of the most challenging conditions. Following are highlights of recent investigations led by Lucian Sulica, MD, Director of the Sean Parker Institute for the Voice, and laryngologists Anaïs Rameau, MD, MPhil, and Babak Sadoughi, MD.
Dr. Anaïs Rameau, Dr. Babak Sadoughi, and Dr. Lucian Sulica
Insight into Pathophysiology of Vocal Fold Lesions
In April 2021, a team from the Sean Parker Institute for the Voice at Weill Cornell Medicine received the American Laryngological Association’s prestigious Casselberry Award for a groundbreaking study that characterizes different patterns of vocal damage from voice use, a phenomenon known as phonotrauma. The Casselberry Award for distinguished contributions to laryngology has only been awarded 27 times in its 105-year history. The Weill Cornell Medicine researchers used information from recurrence of vocal lesions after surgery to build mathematical models of vocal injury that closely predicted observed real-world data.
“For a problem that affects so many patients, surprisingly little is known about phonotrauma. This is the first time we have a solid mechanistic basis to understand the differences in vocal cord lesions caused by this condition,” says Dr. Lucian Sulica, senior author of the study, which was published in the November 2021 issue of The Laryngoscope. Dr. Sulica is also President-Elect of the American Laryngological Association.
Phonotraumatic vocal fold lesions, a subgroup of benign lesions that result from the physical stresses of phonatory vibration, range in appearance and are not easily classified. They include fibrous masses, nodules, podules, polyps, pseudocysts, and others, but factors that account for the differences between them are unclear in light of the fact that they share a common causative factor, namely voice use.
The researchers examined 567 adults operated on by Dr. Sulica for phonotraumatic vocal fold lesions over 13 years in order to determine if recurrence patterns of different lesions revealed the possible mechanisms underlying pathogenesis, and then constructed computer models of vocal fold damage using the information gleaned.
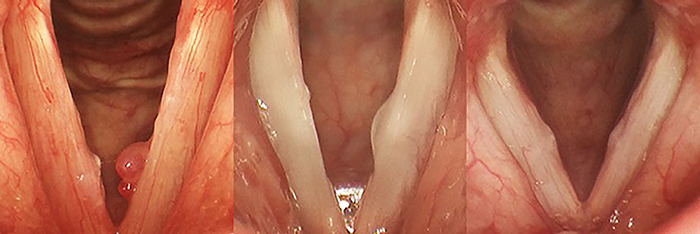
Representative examples of lesion type: (Left) Left-sided polyp (Center) Left-sided pseudocyst (Right) Bilateral midfold fibrous masses (Republished with permission of John Wiley & Sons)
These revealed that some lesions, including vocal fold polyps, recur uniformly over time, suggesting that they arise from sudden tissue reactions to phonotraumatic stress. Others, including pseudocysts, nodules and fibrous masses, tend to recur early and much more often than polyps, suggesting built-in predisposition to cumulative phonotraumatic injury in certain patients.
The researchers at the Sean Parker Institute for the Voice have embarked on further studies to identify those factors that predispose certain individuals to one or the other pattern of phonotrauma. “These may offer a basis to improve the way patients with one or another category of lesions are treated,” says Dr. Sulica.
Read More
Patterns of Recurrence of Phonotraumatic Vocal Fold Lesions Suggest Distinct Mechanisms of Injury. Lee M, Mau T, Sulica L. The Laryngoscope. 2021 Nov;131(11):2523-2529.
A Model Approach for Injection Laryngoplasty Training
“Laryngoplasty is difficult to teach and to learn,” says Dr. Anaïs Rameau. “Advancing the needle through the neck into the throat and directing it in the correct location for the injection does not come intuitively, and patients are also awake during the procedure. Most physicians learn it by trial and error on their own and the patients are very uncomfortable in that process.”
With a limited number of three-dimensionally printed laryngeal simulators available today, and only one designed specifically for percutaneous injection laryngoplasty training, Dr. Rameau set out to develop a low-cost 3D-printed simulator that would improve upon existing models and would be open access. Collaborating with Weill Cornell radiology, the team used CT scans of the upper airways processed with a 3D slicer to generate a computer model of the endolarynx. Computer graphics were used to refine the mucosal model and develop casts for the silicone injection molding. Casted endolaryngeal structures were then inserted into a laryngeal cartilage model.
Assembled laryngeal simulator (Courtesy of Dr. Anaïs Rameau)
Ten expert laryngologists evaluated the final model for its fidelity, educational value, and overall quality, and all reviewers rated it ready for use as is or with slight modifications. The simulator is freely available for download on Wikifactory with tutorials for 3D printing, silicone molding, assembly, and use. The results of the study were published in the March 2021 issue of The Laryngoscope.
“Our next steps are to conduct a randomized control trial and see if it actually improves the skill sets of residents,” says Dr. Rameau.
Read More
An Open-Source Three-Dimensionally Printed Laryngeal Model for Injection Laryngoplasty Training. Lee M, Ang C, Andreadis K, Shin J, Rameau A. The Laryngoscope. 2021 Mar;131(3):E890-E895.
3D Larynx Surgery Trainer. Wickifactory Tutorial.
Vocal Fold Paralysis: Evaluating the Role of Injection Laryngoplasty
Unilateral vocal fold paralysis, which presents with dysphonia, shortness of breath, and difficulty swallowing, results from damage to the recurrent laryngeal nerve generally due to cancers, trauma, or surgery. Swallowing dysfunction is particularly concerning for its risk of aspiration leading to pneumonia and the need for enteral feeding in the immediate postoperative setting. Injection laryngoplasty has become a key component in treatment as a temporary delaying measure and to help improve glottic closure, airway protection, and cough efficiency.
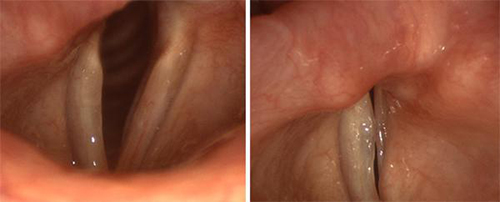
The vocal folds on the left of both images above are paralyzed. Even with extreme effort, they cannot meet their opposing partners.
While injection can improve voice outcomes after paralysis, there is limited information about its potential efficacy in decreasing aspiration. According to Dr. Babak Sadoughi, a laryngologist with the Sean Parker Institute, the indication of injection for aspiration management in iatrogenic unilateral vocal fold paralysis currently relies on anecdotal evidence and empirical practice and thus prompted him to conduct a review of the literature to guide best practice. In a study published in the December 2020 online issue of The Laryngoscope, Dr. Sadoughi sought to determine whether patients with iatrogenic vocal fold paralysis who undergo injection laryngoplasty have improved aspiration outcomes and diet advancement in the early postoperative setting.
The initial in-depth search on several databases yielded 1,590 articles; of that number 92 articles underwent full review by the Weill Cornell investigators. The final qualitative review consisted of 14 case series studies comprising 582 patients with a total of 348 patients treated with injection laryngoplasty for unilateral vocal fold paralysis.
The researchers concluded that the evidence in the literature to support injection laryngoplasty to reduce the risk of aspiration in the acute setting of iatrogenic unilateral vocal fold paralysis was inconclusive. They further note that the indication of injection laryngoplasty for aspiration management continues to rely on empirical practice without validation against control subjects. What is needed are prospective investigations with validated, objective measures to definitively demonstrate the effectiveness of injection laryngoplasty for that indication, as well as support guidelines for timing of interventions.
Read More
Effectiveness of Injection Laryngoplasty for Aspiration in Acute Iatrogenic Vocal Fold Paralysis: A Systematic Review. Pan S, Sadoughi B. The Laryngoscope. 2020 Dec 11. Online ahead of print.
Machine Learning Enhances Diagnostic Capabilities
Dr. Rameau has developed a particular expertise in the use of artificial intelligence (AI) in the diagnostic streamlining of laryngological and swallowing disorders and the application of AI to video laryngoscopy.
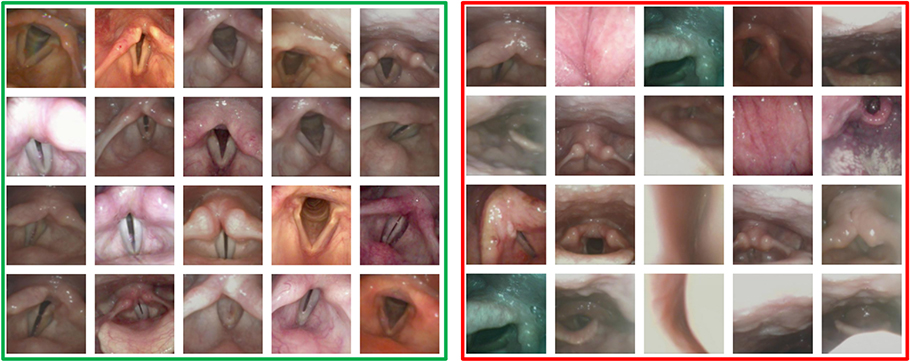
“Laryngologists capture a large number of videos of the larynx and the vocal folds, but there are certain challenges that come with these videos,” says Dr. Rameau. “First, the videos are not static images, unlike radiology or pathology. We have many frames and not all the frames are useful for diagnostics. Another challenge is that the camera is always mobile, thereby not allowing a standard perspective on the structures of the larynx. So, we've been tackling how to extract only those frames that have diagnostic value. With a grant from the American Laryngological Association, over the past year we have developed an algorithm that is able to recognize informative frames among the large number of laryngoscopy videos, basically automating this process, obtaining a precision rate for the recognition of informative frames that is above 80 percent.”
Dr. Rameau has applied the automated algorithm to recognize images of the larynx in patients who have a normal layer and in patients who have a polyp. “We then used this mechanism to recognize the presence of the polyp and again our precision was above 80 percent,” she says. “We’ve been able to not only automate the recognition of informative frames, but we are also currently automating the recognition of abnormal lesions on the vocal fold.”
Informative laryngeal frames (left) versus uninformative laryngeal frames (right)
“We're limited by the number of patients with polyps who come to our center, which does not represent its prevalence across the country,” notes Dr. Rameau, who is collaborating with colleagues in the Department of Otolaryngology – Head and Neck Surgery at NewYork-Presbyterian/Columbia University Irving Medical Center to gain access to a wider range of videos and expanded data sets.
In other AI projects, Dr. Rameau and colleagues at the Sean Parker Institute recently conducted a scoping review for studies on AI and office laryngoscopy in five databases focused on vocal fold vibration analysis, lesion recognition, and vocal fold movement determination. The most frequently automated tasks were recognition of vocal fold nodules, polyp, paralysis, paresis, and cyst. Imaging modalities included high-speed laryngeal videos, stroboscopy, and narrow band imaging endoscopy.
The authors recommended that greater interdisciplinary collaboration among science, technology, engineering, and math (STEM) specialists and otolaryngology research teams can lead to improve demographic reporting and larger and more geographically diverse datasets, which will be critical to future research on AI in office laryngoscopy.
Read More
Applications of Artificial Intelligence to Office Laryngoscopy: A Scoping Review. Yao P, Usman M, Chen YH, German A, Andreadis K, Mages K, Rameau A. Laryngoscope. 2021 Sep 28. [Online ahead of print]
Expanding Access to Specialized Laryngological Care
According to Dr. Rameau, the relatively few number of laryngologists in the United States tend to practice in urban areas, limiting access to this highly specialized field in other parts of the country and indeed the world. “A recurring theme in my research is to try to make some of the high-end subspecialized care available to all.”
To that end, Dr. Rameau and her Weill Cornell colleagues conducted a scoping review to outline disparities research within laryngology to identify gaps in knowledge and guide future research. Of the nearly 5,000 abstracts identified, 51 articles were ultimately included. The most frequently examined condition in relation to disparities was laryngeal cancer, followed by voice disorders, deglutitive disorders, and airway disorders. Sources of inequity ranging from the most common to least common were race/ethnicity, sex/gender, insurance status, geography, income, and education level. No study examined the association of LGBTQ identity with inequity. The researchers concluded that the limited extent of disparities research in laryngology requires further investigation. Results were published in the December 12, 2020, issue of The Laryngoscope.
“Another issue we thought important to address was the availability of voice therapy for patients who are transgender or have a voice that does not match their gender identity,” says Dr. Rameau, who with her Weill Cornell colleagues created Attuned, a free voice and speech coaching iOS app made for the transgender community to support individuals in their exploration and attainment of a voice that matches their gender identity. Funded by the Dean’s Diversity and Healthcare Disparity Research Awards through Weill Cornell Medicine in 2019, the project is a result of the collaboration of Weill Cornell speech pathologists and laryngologists, along with members of the transgender community.
Subsequently, Dr. Rameau with colleagues at Stony Brook University conducted a retrospective consecutive case series of 16 transgender women enrolled in a 12-week gender-affirming voice and communication modification program. Self-reported outcomes and changes in acoustic measures of the voice were found to not always correlate.
“Voice therapy for people transitioning genders is not widely available in the country,” says Dr. Rameau. “Unfortunately, there are a lot of ways that people try to change and modify their voice that is not necessarily healthy. It’s not just a matter of the fundamental frequency or the pitch. There are also components such as resonance, prosody or the pace at which you speak, and also vocabulary. With our app, we offer a comprehensive curriculum with highly detailed videos and exercises that train the user and help them to achieve the gender identity they want to reach with their voice.”
Read More
Healthcare Disparities in Laryngology: A Scoping Review. Feit NZ, Wang Z, Demetres MR, Drenis S, Andreadis K, Rameau A. Laryngoscope. 2020 Dec 12. [Online ahead of print]
Attuned. A voice and speech coaching iOS app for the transgender community.
Outcomes of Gender-Affirming Voice and Communication Modification for Transgender Individuals. Chadwick KA, Coleman R, Andreadis K, Pitti M, Rameau A. Laryngoscope. 2021 Nov 17. [Online ahead of print]