Pulmonary Hypertension: How MRI Can Help Get to the Heart of the Matter
For more than a decade, Jonathan W. Weinsaft, MD, Director, Cardiac MRI Program, NewYork-Presbyterian/Weill Cornell Medical Center, and Pascal Spincemaille, PhD, Associate Professor of Physics Research in Radiology, Weill Cornell Medicine, have been working together to develop new imaging tools to better understand how clinical disorders manifest themselves in myocardial tissue substrate and cardiac physiology. Their achievements have included the development of new MRI tools that provide far higher spatial resolution with the capability of viewing minute structures in the heart. Their collaboration extends to other cardiology subspecialists, radiologists, physicists, and biomedical engineers, forming a team that is bridging basic imaging research with direct applications to patient care.
Working together with heart failure investigators, including Evelyn Horn, MD, Director of Heart Failure and Pulmonary Hypertension at the Perkin Center for Heart Failure, and Jiwon Kim, MD, Associate Director of the Adult Echocardiography Laboratory and Co-Director of the Cardiac MRI Program at NewYork-Presbyterian/Weill Cornell, Drs. Weinsaft and Spincemaille have focused their efforts on the use of new MRI techniques for improved assessment of cardiac structure, function, and tissue properties in patients with heart failure.
In 2021, Drs. Weinsaft, Spincemaille, Horn, and Kim were awarded an R0l grant that is enabling them to build on the pioneering work conducted by Dr. Spincemaille and his colleagues to understand how oxygen, or lack of oxygen, in the heart manifests itself on MRI.
A key manifestation of pulmonary hypertension is impaired oxygenation of the lungs and heart chambers – an index that strongly predicts clinical outcomes but currently requires invasive testing. When pulmonary arterial pressure is increased, pulmonary oxygen exchange suffers, resulting in a decreasing delivery of oxygenated blood to the left heart. Additionally, systemic cardiac output can be compromised leading to a larger differential blood oxygen saturation between the left and right heart.
“Our ultimate goal is to develop a new tool or metric to assess heart function in patients with and without pulmonary hypertension who might otherwise need an invasive catheterization to measure cardiac oxygenation,” says Dr. Weinsaft. “MRI is an important test for evaluating structure and function of the heart but has not been applicable to evaluating blood oxygenation. Imagine if MRI could transcend from a tool that measures size and function to one that can also define physiology. In the last two years, research by Dr. Spincemaille's team has made available to us a whole new dimension in terms of what MRI can assess, enabling me to potentially measure oxygenation in a person's heart without performing a catheterization. I would just place the patient in an MRI scanner.”
“I think that's the strength of this method ,” says Dr. Spincemaille. “MRI is typically used for depicting anatomy, but we have been working on an approach involving magnetic susceptibility – a measure of how a tissue responds to an external magnetic field. While this sounds somewhat esoteric, it has very practical applications. For instance, iron, which has a role in many processes in the body, creates a magnetic susceptibility. The greater the iron content, the greater the magnetic susceptibility. Iron is mostly stored in hemoglobin, which has a different magnetic susceptibility depending on whether it's oxygenated or deoxygenated, which is how we are able to measure deoxygenation in the blood.”
Through a combination of software and advances in MRI technology, Dr. Spincemaille was able to modify in a fundamental way how MRI acquires data to be able to interpret images related to levels of oxygenation. “Deep learning is one of the newer tools that helps us recover the image quality that we can use for diagnosis. AI then enables us to pinpoint relevant parameters such as the difference between oxygen in the left and the right ventricles,” explains Dr. Spincemaille.
MRI: A Novel Approach to Quantifying Oxygen Saturation
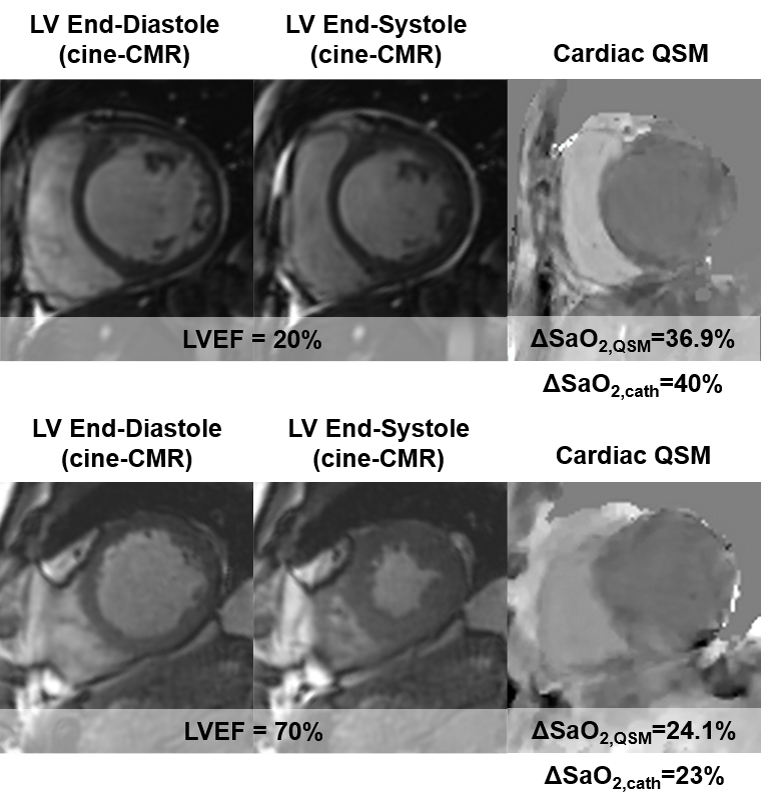
When their research achieved a pivotal milestone with the testing of the new MRI application in selected patients that demonstrated results concurring with those achieved with invasive testing, Dr. Weinsaft and Dr. Spincemaille began transitioning their findings further into the clinic setting.
(Top) Patient with severely reduced LV function (EF=20%); QSM measured marked increase in ΔSa02 (36.9%) similar to invasive catheterization (40%) (Bottom) Patient with normal LV function (EF=70%); QSM measured ΔSa02 (24.1%) similar to invasive catheterization (23%)
Dr. Spincemaille's investigations of MRI were initiated in the brain and other organs before turning to the heart. “It's trickier in the heart because of cardiac and respiratory motion,” notes Dr. Spincemaille. “So, we are using methods that we have developed over the past decade to address this motion as part of the cardiac quantitative susceptibility mapping project funded by NIH. This is a new direction for MRI, reaching beyond obtaining just a graphical depiction to being able to create a map of certain biological properties – in our case oxygenation.”
Developing cardiac quantitative susceptibility mapping (QSM) is not without its challenges, including motion suppression and prolonged scan times. The primary goals of their current research are to develop an accelerated cardiac QSM method and to test the validity of QSM in measuring oxygenation as compared to invasive catheterization. To this end, patients who are scheduled for a catheterization are also asked to undergo non-invasive testing as well. Comparing the data from the two approaches will enable the researchers to determine if cardiac QSM can transform patient management and define its prognostic value.
“I believe cardiac QSM is well-poised to transform patient care,” says Dr. Weinsaft. “Being able to perform a non-invasive oxygenation assessment by this novel technique holds great promise for expediting early diagnosis, optimizing therapy, and improving clinical outcomes for the growing number of patients with pulmonary hypertension.”
Related Publications