Download the Full Report View the E-booklet
Read more about our top research and key innovations from 2025:
Study Finds Spanish-Speaking Sarcoma Patients Face Higher Metastatic Risk
Arthroscopic Approach To Neurogenic TOS May Prevent Rib Resection
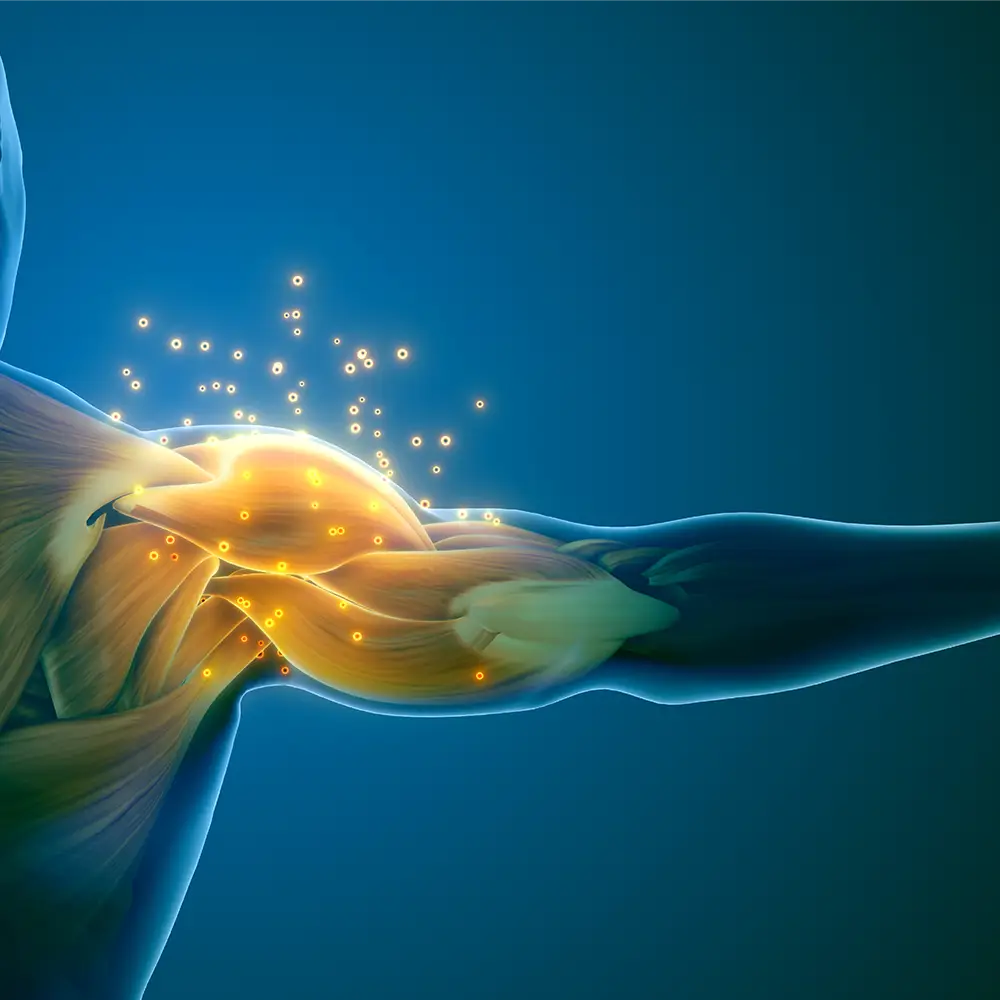
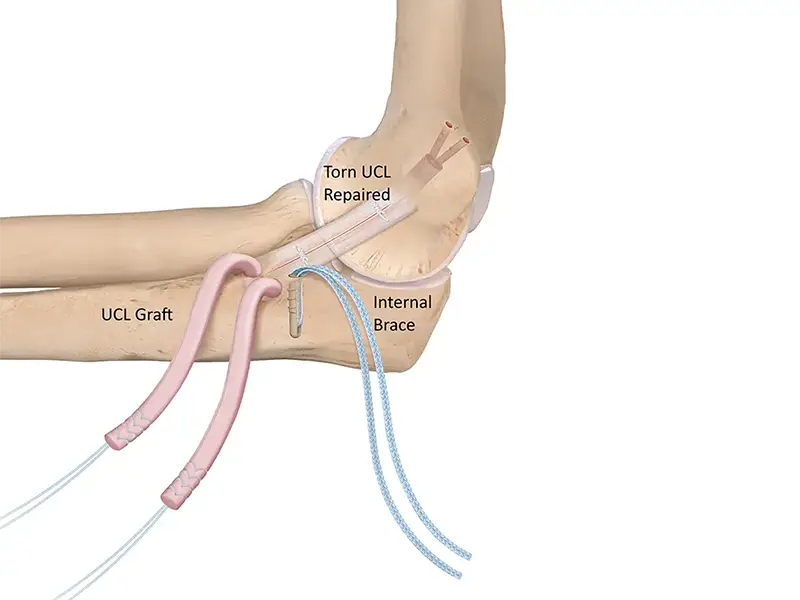
Evolving Tommy John Surgery For Modern Baseball Players
Novel Concussion Biomarker Paves Way For New Diagnostic Tool
Dual-Specialty Approach Improves Outcomes In Pediatric Spine Cases
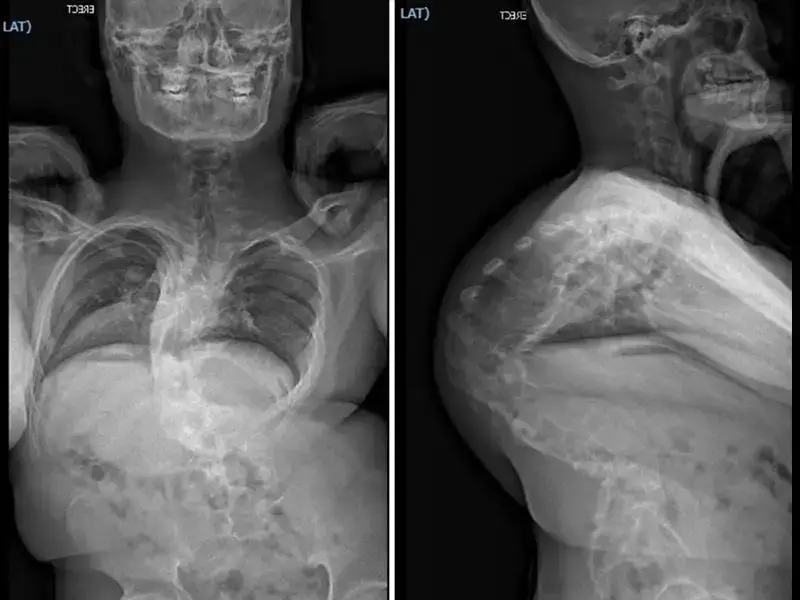
Extensive Multistage Spine Surgery Transforms A Severe Case Of Kyphoscoliosis