Read more about our top research and key innovations from 2024:
Transforming Transplant Medicine with Innovation & Experience
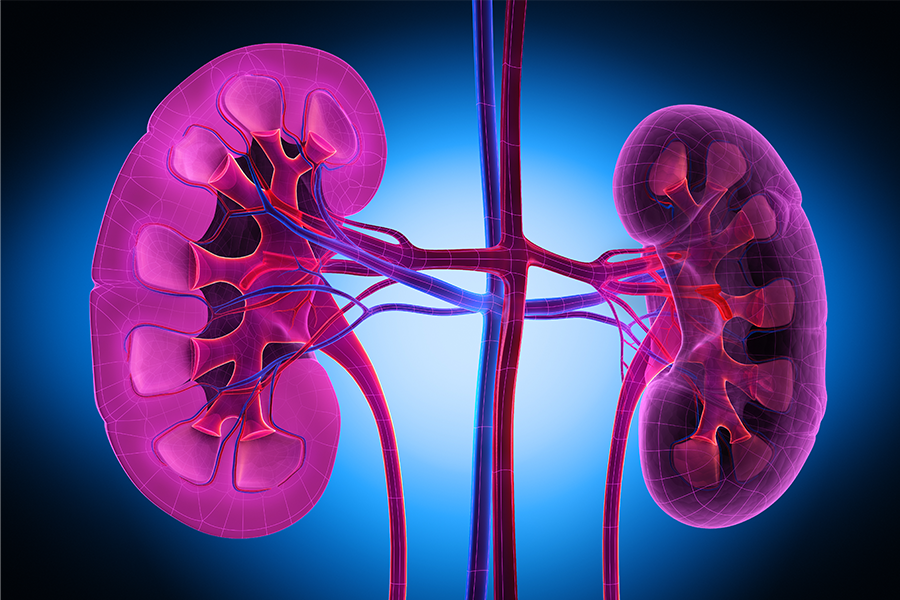
Preserving Kidney Function Through Renal Autotransplantation
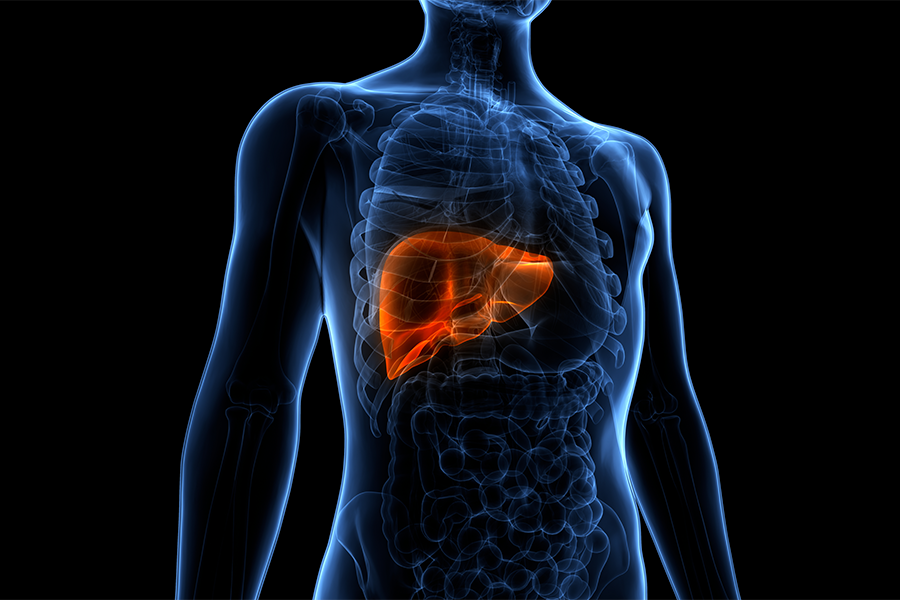
Program Offers Noninvasive Histotripsy for Cancerous Liver Tumors
Reducing Waitlist Mortality for Pediatric Liver Transplant
Reviewing Thirty Years of Pediatric Heart Transplants
Expert Experience: Achieving Greater Success in Lung Transplantation Through Access & Innovation
The Surgical Robot: Advancing Medicine with Robot-Assisted Technology