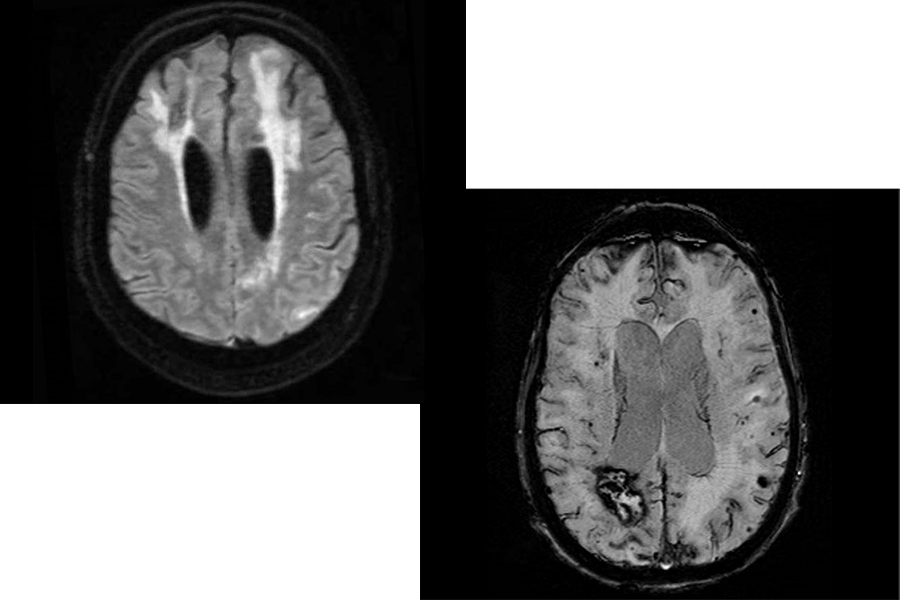
Patients who require surgical intervention for essential tremor typically undergo magnetic resonance-guided focused ultrasound (MRgFUS) thalamotomy in their dominant hand, which provides relief; however patients with bilateral symptoms still experience issues. Michael G. Kaplitt, MD, PhD, executive vice chair of neurological surgery and director of movement disorders and pain neurosurgery at NewYork‑Presbyterian and Weill Cornell Medicine, and Gordon H. Baltuch, MD, PhD, co-chief of functional neurosurgery at NewYork‑Presbyterian and Columbia, collaborated on a multicenter trial treating 51 patients with essential tremor with staged, bilateral MRgFUS thalamotomy. Results from the trial indicated bilateral treatment is generally safe, effective, and can improve functional disability in patients who had already achieved long-term stability in their dominant hand from a previous unilateral procedure. The FDA approved the MRgFUS surgery system for bilateral use, which will change the course of care for patients with these conditions.