NewYork-Presbyterian Hospital is a destination for treatment of complex and challenging musculoskeletal diseases and disorders. Our renowned orthopedic faculty are recognized for their nonoperative and operative approaches to treating sports injuries, spine disorders, degenerative joint and disc diseases, bone and soft tissue cancer, and orthopedic trauma.
NewYork-Presbyterian Hospital’s Columbia orthopedic surgery program – ranked #6 in the country by U.S. News & World Report – is supported by a vibrant research enterprise advancing the field in unprecedented ways.
Understanding the Role of Inflammation in Disc Herniation
Targeting Sarcoma with Greater Precision
Leading the Establishment of Landmark Guidelines in Hip Arthroscopy
Deconstructing Hockey Injuries
Traction or No Traction: That is the Question
Where the Tendon Meets the Bone
Increasing Musculoskeletal Medicine Presence in Medical School

Understanding the Role of Inflammation in Disc Herniation
In a recent multicenter study, Nadeen O. Chahine, PhD, Associate Professor of Biomechanics (in Orthopedic Surgery), Columbia University Vagelos College of Physicians and Surgeons, showed, for the first time, that degree of inflammation is correlated with severity of disc herniation as measured on MRI – a gold standard for herniation diagnosis. The researchers also found that this relationship holds only in patients with chronic symptoms, suggesting that the inflammation is developing over the longer course of herniation. To determine how intervertebral disc disease and subject-specific characteristics contribute to lower back pain, the researchers examined the effects of symptomatic disc herniation and MRI herniation severity on serum cytokine levels in patients. The study provided a better understanding of the inflammatory proteins contributing to pain and disability and the opportunity to develop new therapies for patients with recurring symptoms or who are not candidates for surgery.
MRI images showing two levels of disc disease severity
Targeting Sarcoma with Greater Precision
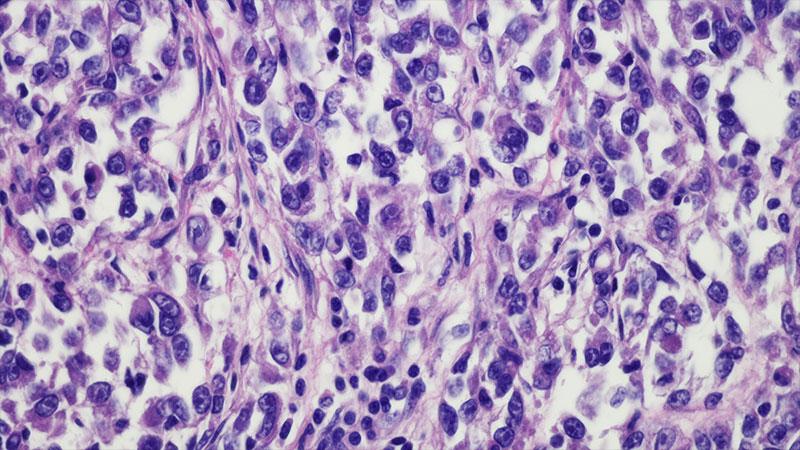
The integrated Sarcoma Service for Cancers of the Bone and Soft Tissues at Columbia is a joint program among physicians in orthopedic oncology, hematology/oncology, and radiation oncology who collaborate on developing the optimal course of treatment for each patient. The therapeutic plan may involve surgery, chemotherapy, radiation and, at times, a combination of all three. Under the leadership of Wakenda K. Tyler, MD, MPH, Chief, Orthopedic Oncology Service, Columbia faculty are involved in gene analysis to identify specific genes that either produce a good response or a poor response to therapy, making it possible for our physicians to determine an alternate therapy with greater precision. Our orthopedic surgeons are also focused on the challenges of diagnosing intra-articular tumors, which are often mistaken for other non-neoplastic conditions, and the importance of recognizing when surgical or nonsurgical treatment is indicated.
Clear cell sarcoma of the leg

Leading the Establishment of Landmark Guidelines in Hip Arthroscopy
Treating chronic hip injuries in the setting of femoroacetabular impingement is particularly concerning because pinpointing the origin of the pain can be difficult as it is not generally linked to a traumatic event. A systematic review and meta-analysis led by Columbia orthopedic surgeon T. Sean Lynch, MD, in collaboration with thought leaders in hip arthroscopy from across the country, has resulted in the establishment of best practice guidelines for the surgical and nonsurgical management of patients with femoroacetabular impingement. The comprehensive tool provides a checklist that can help sports medicine providers, orthopedic surgeons, athletic trainers, and physical therapists deliver optimal and safe care for patients with these athletic hip conditions.
Arthroscopic photo of a hip labral repair

Deconstructing Hockey Injuries
Orthopedic surgeons from the Shoulder, Elbow, and Sports Medicine Service at Columbia undertook a systematic review and meta-analyses of orthopedic injury patterns in professional hockey players over the last 40 years. The physicians summarized and analyzed data on 13,850 players finding that the top injuries involved the hip and pelvis, ankle, and knee, with most injuries occurring in the lower extremities. Injuries were more frequent in games than during practice and more than half of the players missed one game due to injury over the course of a season. The comprehensive review supplies team physicians with a record of literature that may be beneficial in evaluating injury prevention strategies and predicting performance after injury.

Traction or No Traction: That is the Question
Preoperative and/or intraoperative traction may limit postoperative complications associated with growth-friendly instrumentation for early-onset scoliosis (EOS). By gradually correcting the deformity before instrumentation, traction can, theoretically, allow for better overall correction without the complications associated with intraoperative correction. Columbia pediatric orthopedic surgeons Benjamin D. Roye, MD, MPH, and Michael G. Vitale, MD, MPH, led a multicenter study investigating the benefit of traction prior to surgery. The investigators identified 381 patients with EOS who had growth rod instrumentation before 2017. Of these, 57 patients received preoperative traction and 69 patients underwent intraoperative traction. After adjusting for etiology and degree of kyphosis, there was no evidence to suggest that preoperative halo traction reduced the risk of any complication following surgical intervention. This multicenter study provides the best evidence to date of the association between the use of traction and postoperative complications and justifies the need for future studies to characterize the complete benefit and risk profile for traction use in surgical intervention for EOS.
Dr. Michael G. Vitale, Chief, Pediatric Spine and Scoliosis Surgery, Columbia Orthopedics, examines a young patient with early onset scoliosis.
Where the Tendon Meets the Bone
Surgical repair of tendon to bone is plagued by high failure rates largely due to a lack of understanding of how tendon enthesis is formed and maintained. Stavros Thomopoulos, PhD, Director, Carroll Laboratories for Orthopedic Surgery and Vice Chair, Basic Science Research in Orthopedic Surgery at Columbia, continues to study the mechanical, biophysical, and molecular challenges of attaching tendon to bone with a goal of identifying strategies to improve healing.
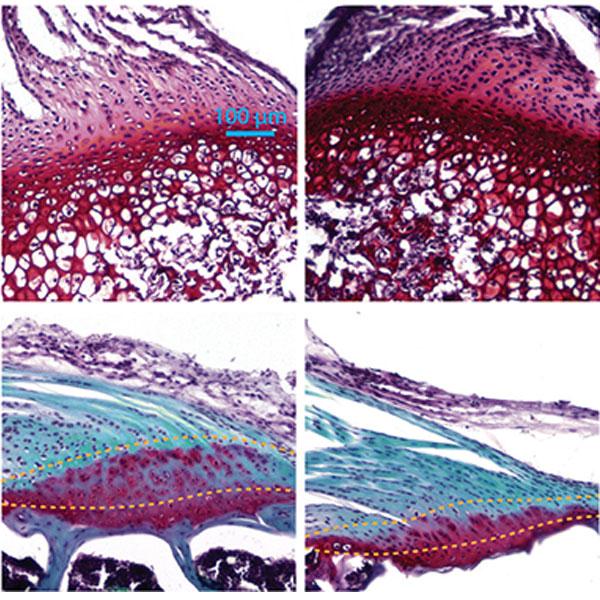
Having previously demonstrated that both mechanical force and Hedgehog (Hh) signaling are essential for tendon enthesis formation, Dr. Thomopoulos and his colleagues recently pursued a study in mouse models of their hypothesis that the primary cilium is a hub for transducing biophysical and Hh signals to regulate tendon enthesis formation and adaptation to loading.
They found that primary cilia were necessary for enthesis development; cilia responded inversely to loading in that increased loading led to decreased cilia and decreased loading led to increased cilia; and that enthesis responses to loading were dependent on Hh signaling through cilia. Their results imply a role for tendon enthesis primary cilia as mechanical responders and Hh signal transducers, providing a therapeutic target for tendon and enthesis pathologies.
Safranin O staining of the tendon entheses from WT and cKO mice at different time points; dashed lines mark the tendon enthesis.

Increasing Musculoskeletal Medicine Presence in Medical School
Leaders of the Columbia Orthopedics Residency Training Program – Charles M. Jobin, MD, Residency Program Director; T. Sean Lynch, MD; and William N. Levine, MD – recently examined deficiencies in medical student knowledge in musculoskeletal medicine, including current curriculum and technology practices. They found that only 15 percent of medical school programs have musculoskeletal disease curriculum and less than 50 percent of students applying for orthopedic surgery programs have the prerequisite anatomic knowledge before entering residency. They suggest that the use of effective teaching modalities, such as additional lectures, anatomy sessions, and focused small group learning, along with new teaching platforms such as 3D software, podcasts, near-peer learning in-person and electronically, have laid the foundation for future education initiatives at Columbia with the potential for developing similar curriculum and teaching models at other medical colleges.
Dr. Charles M. Jobin



