Adult Spine
NewYork-Presbyterian Och Spine Hospital
Three years ago, NewYork-Presbyterian launched a spine hospital with the guiding principle of providing, under a single roof, a world-class center to treat the full range of conditions that can affect the spine. The NewYork-Presbyterian Och Spine Hospital, located at NewYork-Presbyterian Allen Hospital, has emerged as a destination for an increasing number of patients coming from around the world with complex and challenging spinal problems. Here, they find an integrated approach that unites the expertise of orthopedic spinal surgeons, neurosurgeons, physiatrists, pain management specialists, physical therapists, and specialized nursing staff.
Renowned Leadership and Expert Surgical Team
Lawrence G. Lenke, MD, Surgeon-in-Chief of the NewYork-Presbyterian Och Spine Hospital; K. Daniel Riew, MD, Director of Cervical Spine Surgery; and Ronald A. Lehman, Jr., MD, Director of Degenerative and Minimally Invasive Spine Surgery, oversee this singularly focused endeavor for spinal care. The surgical team is trained in the most advanced, least-invasive surgical techniques, including microsurgical and minimally invasive options.
For the most complex spinal deformity surgeries, our surgeons employ CT imaging data to create 3D models in order to precisely plan the placement of screws and other aligning techniques before and during surgery. Patient care is coordinated with NewYork-Presbyterian’s hospitalists, intensivists, cardiologists, endocrinologists, pulmonologists, and other specialists to optimize surgical outcomes and expedite recovery.

Dr. Lawrence G. Lenke

Dr. K. Daniel Riew

Dr. Ronald A. Lehman, Jr.
Outcomes and Quality Metrics
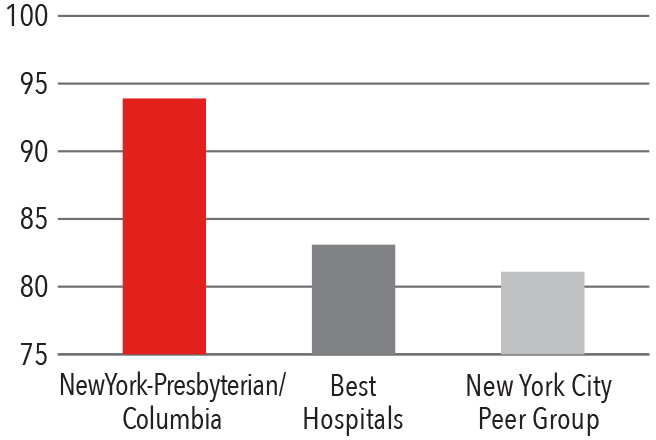
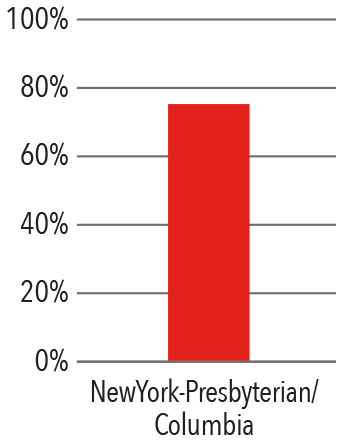
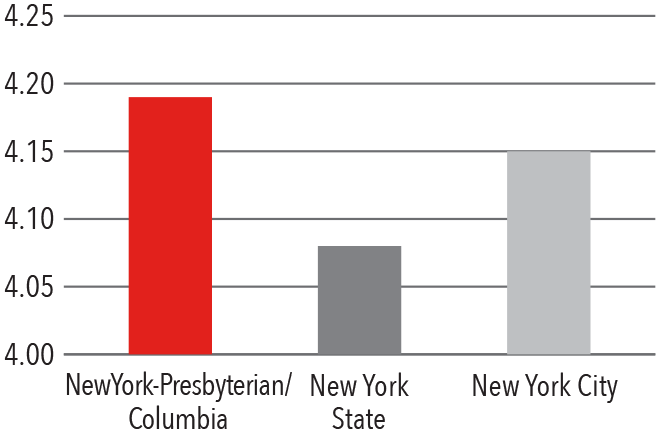
Patient Satisfaction 2016 - 2017
HCAHPS Communication with Doctors
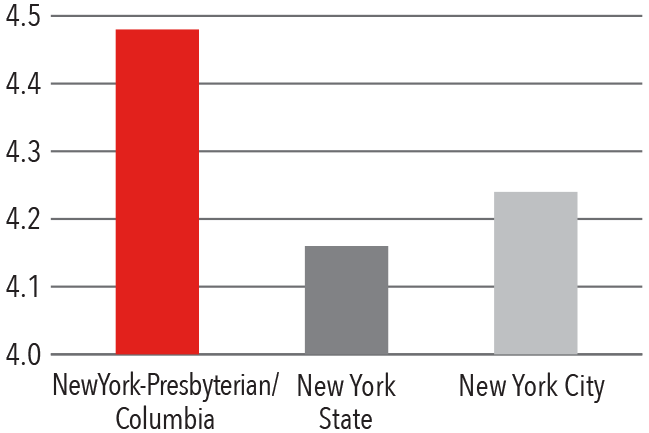
Press Ganey Physician Score
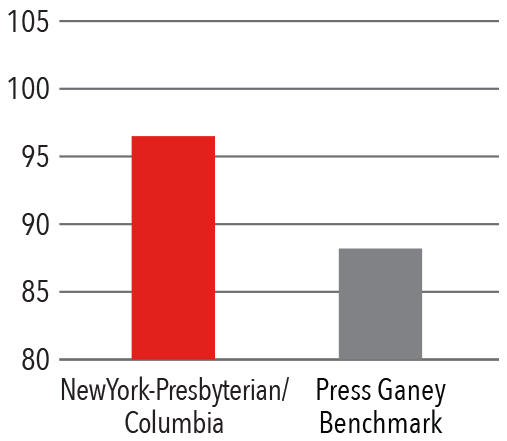
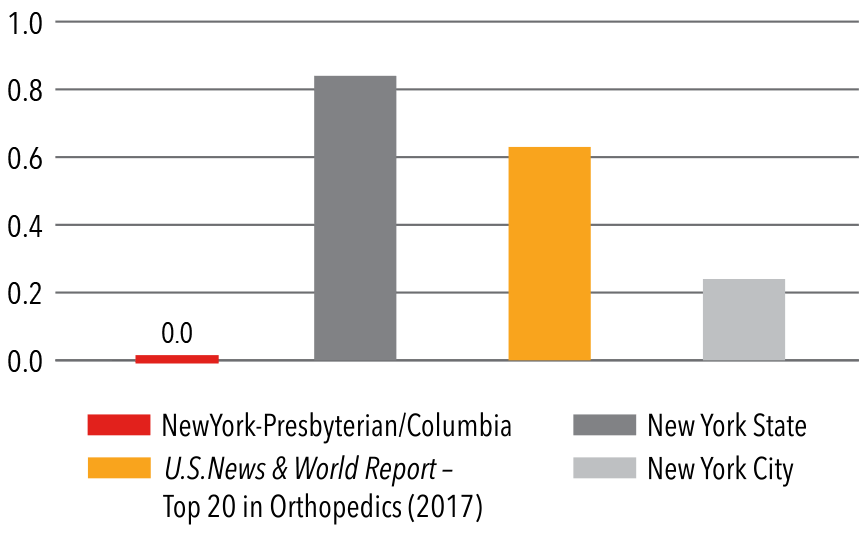
Compared to New York State and New York City hospitals, Columbia spine surgeons treat a more complicated, comorbid, and high-risk patient population.
Clinical Quality 2016 - 2017
Optum Survey - 2016
Deep Vein Thrombosis Rate
Patients Discharged Home
Case Mix Index Medicare
Case Mix Index Non-Medicare
Advanced Robotic Technologies
Robotic technology is used by our spinal surgeons to enhance positioning accuracy, minimize invasiveness, and reduce radiation exposure to the patient and surgical team during spine surgeries. The bone-mounted, miniature robotic system guides the accurate placement of implants, offering surgical tool guidance while leaving the actual procedure in the surgeon’s hands.
Dedicated Spine Facilities
The surgical suites are designed explicitly for spinal procedures with attention placed on optimal patient positioning, while also providing appropriate access for anesthesia, the spinal cord/nerve root monitoring team, as well as intraoperative CT scans, X-rays, and fluoroscopy, all with an eye towards reducing complications. These facilities include:
-
2 operating rooms custom built for spine surgeries
-
Low radiation EOS X-ray imaging and 3D computed tomography
-
Robotics system
-
Real-time OR video feed to surgery observation rooms
-
ICU beds attended by spine-specific intensivists
Case Study Neurofibromatosis and Thoracic Kyphoscoliosis
A 23-year-old male who had neurofibromatosis and severe thoracic kyphoscoliosis complained of back pain and some shortness of breath along with preoperative right leg pain in his posterior thigh and calf. He presented with some lower extremity weakness and a spastic gait. The patient was in halo gravity for two months for a severe deformity greater than 180 degrees of kyphoscoliosis. Following the halo traction, the patient was treated with a posterior spinal instrumentation and fusion from T1-L4 and is now doing well.

BeforeAfter
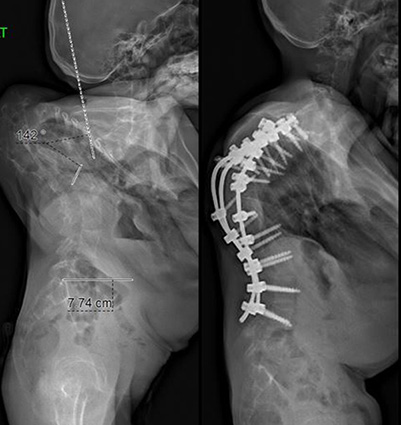
BeforeAfter
Advancing Spine Care
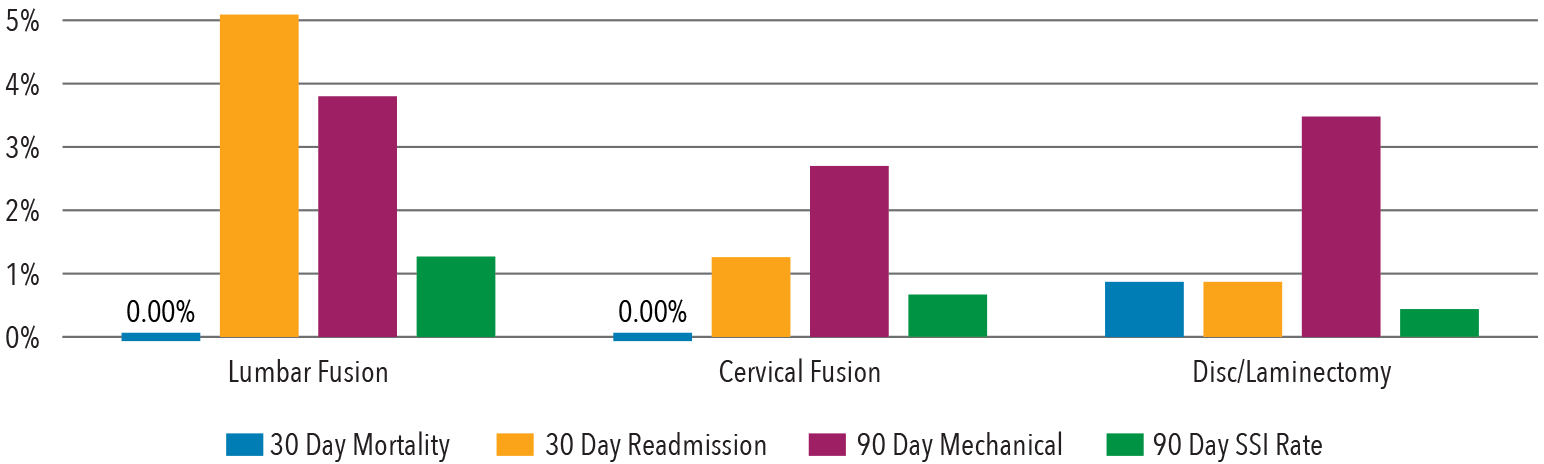
Update: Postoperative Surgical Site Infection After Spine Surgery
Despite advancements in surgical technique and infection prophylaxis, postoperative surgical site infection (SSI) remains one of the most common complications in spinal deformity surgery. In the November 2018 issue of Spine Deformity, Columbia spine surgeons presented their analysis of the incidence and characteristics related to postoperative SSI using the Scoliosis Research Society Morbidity and Mortality database. The researchers found that SSIs occurred in 1.2 percent of spine deformity patients, with a rate significantly higher in patients with kyphosis. Approximately 25 percent of these infections were secondary to gram-negative species. Antibiotic complications occurred in 4.5 percent of patients being treated for SSI. Future studies are necessary to further elucidate potentially modifiable preoperative risk factors and develop evidence-based treatment protocols for the management of postoperative SSI.
Infection Complication Rates
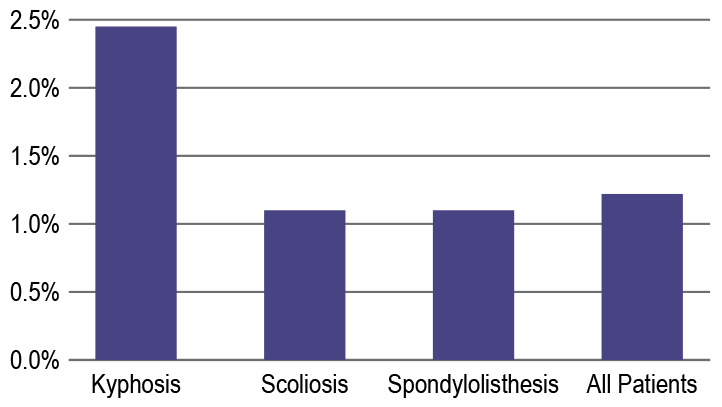
Infection complication rates were compared based on diagnosis.
The rate of postoperative SSI varied based on the spinal pathology.
(Source: Spine Deformity, Volume 6, Issue 6, November-December 2018)
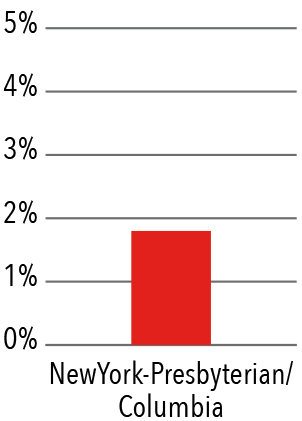
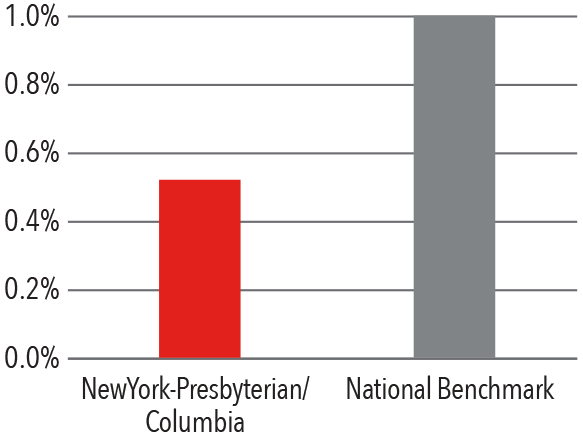
Outcomes and Quality Metrics
Clinical Quality 2017
Surgical Site Infection Rate
Mortality Index
AOSpine-SRS Scoli-RISK-1 Study

Dr. K. Daniel Riew
The landmark Scoli-RISK-1 study evaluating the neurologic complications associated with surgical correction of complex adult spinal deformity (ASD) published its two-year results in The Journal of Bone & Joint Surgery in October 2018. Dr. Lawrence Lenke served as Co-Principal Investigator of the study — an example of a successful academic collaboration between two leading societies — the Scoliosis Research Society (SRS) and AOSpine. For the first time, the prospective multicenter observational study included formal neurologic assessment of patients undergoing complex ASD surgery. The 15 participating clinics from North America, Europe, and Asia collected information on all complications and patient-reported outcomes from 272 patients. Data was collected before surgery and at various timepoints after surgery up to two years postoperative. “The rate in neurologic decline was much higher than expected, which gives us a baseline to work off to lower the rate of complication,” says Dr. Lenke. At two years post surgery, more than half the patients had improved their neurologic weakness or deficits.
Dr. Lawrence Lenke served as Chairman of the 4th Annual International Spinal Deformity Symposium (ISDS) in November 2018 and as Co-Chairman at Broadwater’s Spine: Base to Summit Meeting in January 2019.
Spine Study Team Wins Prestigious Whitecloud Award
Dr. Lawrence Lenke, along with J. Alex Sielatycki, MD, Comprehensive Spine Fellow; Eduardo Beauchamp, MD, Advanced Pediatric Spinal Deformity Fellow; and Meghan Cerpa, MPH, Research Coordinator, have won the prestigious Thomas Whitecloud Award at the 2018 International Meeting on Advanced Spine Techniques (IMAST). The award was presented for their paper, “The Relative Curve Correction is More Important than UIV Selection for Shoulder Balance in Lenke Type 1 and 2 AIS.”
Novel Integrated Spine Fellowship Established
In August 2018, the Department of Orthopedic Surgery welcomed both orthopedic and neurosurgery fellows into the recently integrated orthopedic and neurosurgery spine fellowship program, providing formal rotations with both Columbia Orthopedics and Neurosurgical spinal surgeons. The one-year fellowship offers training in all aspects of the cervical, thoracic, and lumbar spine, from degenerative diseases and deformity to trauma injuries and tumors. Fellows perform surgical cases that include complex scoliosis and kyphosis corrections with three-column osteotomies and minimally invasive procedures for cervical and lumbar disc disease.



