Expanding Minimally Invasive Gynecologic Surgery Services
Dr. Ja Hyun Shin, Director of Minimally Invasive Gynecologic Surgery, NewYork-Presbyterian/Weill Cornell Medical Center
The Department of Obstetrics and Gynecology at NewYork-Presbyterian/Weill Cornell Medical Center has welcomed Ja Hyun Shin, MD, as Director of Minimally Invasive Gynecologic Surgery. Dr. Shin, an expert in advanced laparoscopic and robotic procedures, is dedicated to providing women with the least invasive but most effective treatment options, including both surgical and non-surgical approaches.
In her new role, Dr. Shin is building upon the expertise already available in the Division of Minimally Invasive Gynecologic Surgery at Weill Cornell, which now has a team of five gynecologic surgeons. “I am thrilled to join a world-class surgical team and be a part of this extraordinary OB/GYN department.” With the support of Laura Riley, MD, Obstetrician and Gynecologist-in-Chief at NewYork-Presbyterian/Weill Cornell and Chair of the Department of Obstetrics and Gynecology at Weill Cornell Medicine, and Kevin Holcomb, MD, Vice Chair of Gynecology, Weill Cornell Medicine, the Division of Minimally Invasive Gynecologic Surgery has established several multidisciplinary treatment programs to advance gynecologic care and surgical options for women.
“Our specialty is dedicated to safely treating women who suffer from gynecologic conditions that may at times require complex surgeries by the most minimally invasive route,” says Dr. Shin. “Our expert surgeons perform laparoscopic and robotic procedures for the most challenging of cases. As a division, we seek to expand minimally invasive treatment options for our patients. This can include multidisciplinary collaborations that lead to a novel approach to improve surgical outcome, or offering the newest advances in surgical technology such as radiofrequency ablation for fibroid treatment.”
“Our expert surgeons perform laparoscopic and robotic procedures for the most challenging of cases. As a division, we seek to expand minimally invasive treatment options for our patients. This can include multidisciplinary collaborations that lead to a novel approach to improve surgical outcome, or offering the newest advances in surgical technology such as radiofrequency ablation for fibroid treatment.” — Dr. Ja Hyun Shin
“The benefits of minimally invasive surgeries are well known, including decreased postoperative pain and recovery time, so that women can get back to their normal routine quickly and in the most comfortable way possible,” continues Dr. Shin. “We also discuss nonsurgical options as well, depending on what would lead to the best outcome for the patient. It’s important that as surgeons, we not only offer our surgical expertise, but also provide comprehensive information on current medical and procedural treatments so that patients can be fully empowered to make the right decision along with their doctors.”
Dr. Shin and the Weill Cornell Minimally Invasive Gynecologic Surgery team specialize in the diagnosis and treatment for the full range of gynecological disorders, including adenomyosis, endometriosis, uterine fibroids, ovarian cysts, pelvic pain, and abnormal uterine bleeding. Procedures commonly performed include laparoscopic and robotic surgeries for endometriosis excision, myomectomy, and hysterectomy. They are also equipped to perform office hysteroscopy procedures for diagnostic purposes and some treatments for patients who otherwise could avoid going to the operating room.
“We continuously strive to safely push the envelope in terms of which patients with which conditions are appropriate candidates for minimally invasive techniques,” says Dr. Shin. “We have state-of the-art facilities and the most up-to-date instrumentation to help maximize technical ability for a variety of gynecologic procedures.”
Fibroid and Adenomyosis Program: Collaborative and Comprehensive
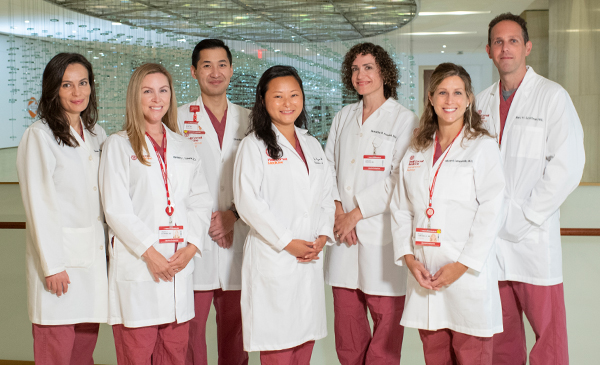
Dr. Yelena Havryliuk, Dr. Kimberly L. Scherer, Dr. Bradley Pua, Dr. Ja Hyun Shin,
Dr. Tamatha B. Fenster, Dr. Nicole Lamparello, and Dr. Marc Schiffman
One of Dr. Shin’s first priorities since her arrival has been to establish a Fibroid and Adenomyosis Program with a multidisciplinary collaboration among specialists in minimally invasive gynecologic surgery and interventional radiology. In addition to Dr. Shin, the team includes minimally invasive gynecologic surgeons Tamatha B. Fenster, MD, Yelena Havryliuk, MD, and Kristen Pepin, MD, and vascular interventional radiologists Nicole Lamparello, MD, Kimberly L. Scherer, DO, and Marc Schiffman, MD – all of whom work closely together to offer patients a range of innovative therapies tailored to their specific condition, symptoms, and reproductive goals.
“The Program creates a streamlined approach to improve access to all options for fibroid management while also considering patient convenience and specific goals,” adds Dr. Shin. “We help patients decide what the best option is for them and their health, lifestyle choices, and reproductive plans. This involves the collaboration among multiple specialties. For each patient that may need to undergo a complex treatment, including surgery, we meet as a group and discuss every aspect of care and come up with the best plan. That is what makes our program so special – every patient is going to get individualized care.” Dr. Lamparello oversees monthly conferences to facilitate these discussions, review imaging findings, and monitor performance metrics.
Dr. Havryliuk stresses that counseling the patient beforehand is integral to the treatment process. “If the patient has fibroids or adenomyosis, we have the ability through the Program to offer consultations with various experts on that same appointment day. Where it might take three or four appointments and several weeks or even months to see all the specialists elsewhere, we have all the specialties on site to help patients efficiently decide on a treatment path that is right for them. We make it easy and convenient.”
Another unique feature of the Program is the capability to coordinate ultrasound and MRI appointments for the same day as the patient appointment, as well as telemedicine consultations. “These efforts are important and necessary to avoid multiple visits to the hospital during this unprecedented time when patient safety is our priority,” says Dr. Shin.
A Focus on Innovation
“The Fibroid and Adenomyosis Program is also a hub of innovation, a place where creative minds in gynecology and interventional radiology, are at the forefront of advancing biomedical technology. We also collaborate with experts in reproductive endocrinology and a network of specialists in pelvic floor dysfunction, physical therapy, and integrative medicine – all under one roof – to provide the best possible care for our patients,” says Dr. Fenster. “Today’s cutting-edge, surgical innovations enable us to take out enormous tumors and let patients go back to their jobs and life within a mere number of weeks.
“The Fibroid and Adenomyosis Program is a hub of innovation, a place where creative minds in gynecology and interventional radiology are at the forefront of advancing biomedical technology.” — Dr. Tamatha B. Fenster
Dr. Fenster continually seeks the latest technologies to further refine minimally invasive surgery. She established office-based hysteroscopy in her practice and is a specialist in single-port laparoscopic surgery. Most recently she created a vaginal retractor, a novel tool to improve patient comfort during office-based procedures. “My whole mission is getting patients back to their routine as soon as possible, so if I can accomplish a surgery in the office with a paracervical block, then that’s what I want to do,” she says. “The field is constantly evolving, so creating new technology and investigating newer and safer technology has to be the foundation of my work.”
“There’s an important role for the gynecologist and the interventional radiologist to work together in determining which patients should benefit from which procedures,” adds Dr. Schiffman, who is broadly trained in interventional radiology, including peripheral vascular disease and neuro-interventional procedures. “Having a facile dialogue discussing cases together is an important step in making sure that we optimize care.”
Very often the physicians collaborate on surgeries, each bringing a specific skill set to provide optimal treatment. For example, for fibroids traditionally deemed too large for a minimally invasive approach and at increased risk for significant blood loss during surgery, Dr. Schiffman will first embolize the fibroid and Dr. Fenster then steps in to remove the tumor laparoscopically. “We have such a good working relationship that we often review cases together, refer back to each other, and then on occasion do these combination procedures,” says Dr. Schiffman. “What is unique about the Fibroid and Adenomyosis Program is our willingness to work with patients to meet their desires and goals. So many patients have been told that they had to have a hysterectomy. But working with the gynecologists here, we respect the patient’s wishes and try to figure out safe, less-invasive options for them.”
It was during these types of collaborations that an integrated fibroid treatment center was envisioned. “This approach would allow us to maximize minimally invasive surgery by controlling the blood supply first,” adds Dr. Fenster. “To us, a fibroid center was a natural extension of that collaborative concept.”
Encouraging the Embolization Option
Dr. Schiffman has successfully performed a high volume of uterine artery embolization cases and is quick to dispel the notion that embolization only works a small percentage of the time. “We have randomized controlled data comparing embolization, which is an outpatient procedure and does not require general anesthesia, to surgery,” says Dr. Schiffman. “The data show that this can be a highly effective procedure with low complication rates and allows for a fast recovery and return to work – about one week following embolization versus two to three weeks with laparoscopic or robotic surgery or six to eight weeks with open surgery.”
One of Dr. Schiffman’s goals is to increase awareness of embolization as a first-line treatment for uterine fibroids. “According to the American College of Gynecology, there are three first-line procedures for patients with uterine fibroids: embolization, myomectomy, and hysterectomy, depending on the context. And despite ACOG reporting all patients should be informed about embolization as a treatment option, there are much less-effective procedures that are not first-line still being done much more frequently than embolization. This is further supported by research by the Society of Interventional Radiology that found only about 40 percent of patients are actually told about embolization. In my experience, less than 30 percent of patients are told.”
“According to the American College of Gynecology, there are three first-line procedures for patients with uterine fibroids: embolization, myomectomy, and hysterectomy, depending on the context. That being said, a research investigation by the Society of Interventional Radiology showed that only about 40 percent of patients are actually told about embolization as an option.” — Dr. Marc Schiffman
Dr. Schiffman notes there are very few patients who are not candidates for embolization. “This is particularly the case if we work together with the gynecologist,” he says. “We can also offer embolization to women at menopause who have symptoms other than bleeding. Many of our patients have suffered with fibroids for years but delayed getting treatment to avoid surgery unaware that minimally invasive options were available. And while bleeding symptoms typically resolve during menopause, frequently fibroids continue to cause discomfort due to uterine size. For women in menopause, I can use embolization to shrink the uterus between 30 to 60 percent, and in some cases up to 80 percent. Adenomyosis is another condition that could be managed with embolization. It can cause very similar if not identical symptoms to patients with fibroids and we are able to offer embolization for this condition as well.
Uterine-Sparing Alternatives
Dr. Havryliuk is among the few physicians in the tri-state area to perform the Acessa procedure, an alternative to hysterectomy and myomectomy. This minimally invasive laparoscopic technique delivers radiofrequency energy to destroy the fibroids. After treatment, the fibroids are reabsorbed by the surrounding tissue. Acessa allows the surgeon to treat only the fibroids, while preserving normal function of the uterus.
“If a patient has fibroids or adenomyosis, we have the ability through the Program to offer consultations with various experts on that same appointment day. Where it might take three or four appointments and several weeks or even months to see all the specialists elsewhere, we have all the specialties on site to help patients decide on a treatment path that is right for them. We make it easy and convenient.” — Dr. Yelena Havryliuk
“We insert an ablation needle inside the fibroid and confirm the placement via laparoscopic ultrasound,” says Dr. Havryliuk. “We then activate the heating cycle that destroys the fibroid via a process of coagulative necrosis. Over time that fibroid softens and shrinks down in size. We do multiple hits to make sure we addressed the entire volume of the fibroid and then move on if the patient has multiple fibroids. This is a very direct treatment of the fibroid and doesn’t affect the ovarian reserve.”
“The fibroid takes about three months to shrink, which is when most patients notice significant improvement in their symptoms,” continues Dr. Havryliuk. “Another advantage of the laparoscopic radiofrequency ablation procedure is that by doing a laparoscopy we can potentially see if the patient has other pathologies that we can treat at the same time.”
Another uterine-sparing procedure is MRI-guided focused ultrasound. “This technique is a completely non-invasive approach that we are also able to offer patients,” adds Dr. Schiffman. “Patients lie in the MRI gantry, and I can aim an ultrasound beam through the skin, which heats up and destroys the fibroid tissue. We can then move to another site during the same procedure. There are not many places across the country that offer this technology within the MRI magnet.”
Facilitating Research
“Our radiologists and surgeons are compassionate physicians dedicated to patient care and also committed to improving and expanding knowledge of gynecologic diseases and treatments through research efforts,” says Dr. Shin. “In the past few years we have individually and collaboratively published our work in numerous peer-reviewed journals. These topics include innovative approaches to fibroid treatment and related complications, pain management after minimally invasive hysterectomies, and systematic reviews and updates of the current available evidence for fibroid management.
Dr. Shin and her team are currently creating a fibroid data repository for clinical outcomes research. “We’re hoping this database will ultimately contribute to patient education and to the medical community in a meaningful way,” says Dr. Shin.
Dr. Shin sits on several expert panels related to fibroid management and developing best-practice recommendations. “I currently serve on the Practice Committee of the American Association for Gynecologic Laparoscopists and we are reviewing the surgical and interventional literature for fibroid management in advance of creating a consensus statement,” says Dr. Shin, who trains other surgeons in these procedures during national and international conferences.
Dr. Shin is also a member of the Society of Interventional Radiology Uterine Artery Embolization Practice Guidelines Committee. “This is an exciting opportunity to collaborate with national experts on fibroid treatments to create guidelines for uterine artery embolization practices and address areas where there may be gaps in information about treatment efficacy, fertility related issues, and comparison to surgery and other procedures,” says Dr. Shin.
Endometriosis and Pelvic Pain Program: A Multifaceted Approach
Dr. Lona Prasad, Dr. Ja Hyun Shin, and Dr. Kristen Pepin
Among the specialized services offered within the Division is the Endometriosis and Pelvic Pain Program. “We recognize that our patients and this disease are multifaceted,” says Dr. Shin. “Given the complex nature of endometriosis and related pain conditions, we have a multidisciplinary team comprised of specialists in minimally invasive surgical techniques, pain management, and pelvic floor disorders to treat all aspects of a patient’s health and well-being affected by endometriosis and pain. We also collaborate with Integrative Medicine physicians who take a holistic approach to patient care that include therapies such as mindfulness, body movement, acupuncture, nutritional and behavioral counseling. This level of coordinated care is unique.”
“We are very aware that many of our patients who come to us with endometriosis have had sometimes almost a decade of delayed diagnosis and have had a very long journey to get the appropriate care. Our goal is to give them the answers and treatment they need to live a life without debilitating pain from endometriosis.” — Dr. Ja Hyun Shin
As Dr. Shin explains, endometriosis can be a complex disease with symptoms that often require surgery in conjunction with medical therapies. “Our gynecologists are able to thoroughly counsel our patients on all treatment options, including surgery for advanced stage endometriosis, which we can successfully treat by a minimally invasive approach,” she says. “We are very aware that many of our patients who come to us with endometriosis sadly have had sometimes almost a decade of delayed diagnosis and have had a very long journey to get the appropriate care. Our goal is to give them the answers and treatment they need to live a life without debilitating pain from endometriosis.”
The program also addresses other chronic pelvic pain conditions, such as painful bladder syndrome, myofascial abdominal wall pain, pelvic floor tension myalgia, and functional bowel disorders. “We are one of the only centers in New York with women’s health experts in all these areas,” notes Dr. Shin. “These conditions are important to recognize and treat because many of them go hand in hand with endometriosis. Our goal for each patient is to accurately and efficiently diagnose endometriosis and other pelvic pain conditions and develop a targeted treatment plan that takes into account each patient’s symptoms and goals for their health and well-being.”
About Dr. Ja Hyun Shin
Dr. Shin completed her residency in obstetrics and gynecology at NewYork-Presbyterian/Columbia University Irving Medical Center. She completed a fellowship in minimally invasive gynecologic surgery at the University of Rochester Medical Center and advanced training in robotic surgery at Albert Einstein College of Medicine/Montefiore Medical Center, after which she joined the Division of Minimally Invasive Gynecologic Surgery. At Montefiore Medical Center, Dr. Shin served as the Director of Pelvic Pain and Multidisciplinary Resident Robotic Training and was the Associate Director of the Minimally Invasive Gynecologic Fellowship Program. Within these roles, Dr. Shin focused on the education and training of residents, fellows, and faculty in performing safe minimally invasive surgeries.
Dr. Shin is committed to practicing evidence-based medicine and providing her patients with the most current information to optimize the decision-making process. She serves on numerous national committees within the American Association of Gynecologic Laparoscopists, Society of Interventional Radiology, and as a Board member of the Society for Laparoscopic and Robotic Surgeons. Dr. Shin is dedicated to research activities to help establish best practice guidelines, improve surgical techniques, and reduce surgical complications.
For more information
Weill Cornell Medicine Fibroid and Adenomyosis Program
To schedule an appointment, call 646-962-4100
https://weillcornell.org/the-weill-cornell-medicine-fibroid-and-adenomyosis-program
Weill Cornell Medicine Endometriosis and Pelvic Pain Program
To schedule an appointment, call 212-746-3171
https://weillcornell.org/endometriosis-and-pelvic-pain-program-at-weill-cornell-medicine