NewYork-Presbyterian High-Risk Obstetrics and Neonatal Care 2018 Clinical and Scientific Innovations Highlights
NewYork-Presbyterian High-Risk Obstetrics and Neonatal Care
-
Neonatology program ranks #8 in the nation by U.S.News & World Report
-
NewYork-Presbyterian ranks in more pediatric specialties than any other New York metro area hospital in U.S.News & World Report’s "Best Children’s Hospitals"
-
Designated as a Regional Perinatal Center by the State of New York, the highest hospital classification level
-
Two Level IV Neonatal Intensive Care Units
-
ECMO program designated by the Extracorporeal Life Support Organization as a Platinum Center of Excellence in Life Support
-
Network Center of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network
Dear Colleague:
We are pleased to bring you highlights from our 2018 Report on Clinical and Scientific Innovations in High-Risk Obstetrics and Neonatal Care at NewYork-Presbyterian. During the past year, NewYork-Presbyterian – in collaboration with our distinguished medical schools, Columbia University Vagelos College of Physicians and Surgeons and Weill Cornell Medicine – continued to build on the strengths of its many clinical and research endeavors to advance care for pregnant women who may be at risk for a premature or complicated delivery and their newborns.

Mary E. D’Alton, MD
Director of Services
NewYork-Presbyterian Sloan Hospital for Women
Chair, Obstetrics and Gynecology
Willard C. Rappleye Professor of Obstetrics and Gynecology
Columbia University Irving Medical Center

Laura E. Riley, MD
Obstetrician and Gynecologist-in-Chief
NewYork-Presbyterian/Weill Cornell Medical Center
Chair, Obstetrics and Gynecology
Professor of Clinical Obstetrics and Gynecology
Weill Cornell Medicine

Jeffrey M. Perlman, MB, ChB
Chair, Newborn Medicine
NewYork-Presbyterian Komansky Children’s Hospital
Professor of Pediatrics
Weill Cornell Medicine

Richard A. Polin, MD
Director, Neonatology
NewYork-Presbyterian Morgan Stanley Children’s Hospital
Vice Chair, Academic and Clinical Affairs, Pediatrics
William T. Speck Professor of Pediatrics
Columbia University Irving Medical Center
For More Information
Measures of Distinction
Clinical Care
-
29 Maternal-Fetal Medicine Specialists
-
39 Neonatologists
-
112 NICU Bassinets
-
17 Infant Cardiac ICU Bassinets
-
143 Neonatal (<30 days) Cardiac Surgery Procedures
Specialized Programs
-
Maternal-Fetal Medicine
-
Preterm Birth Prevention Center
-
Neonatology-Perinatology
Graduate Medical Education
-
49 residents in obstetrics and gynecology
-
18 fellows in maternal-fetal medicine
-
39 fellows in neonatolgy-perinatology
Innovations at a Glance
-
Constructing the NewYork-Presbyterian Alexandra Cohen Hospital for Women and Newborns, a first-of-its kind, state-of-the-art hospital in the region, which will include 60 neonatal intensive care bassinets and 20 maternal critical assessment treatment rooms

-
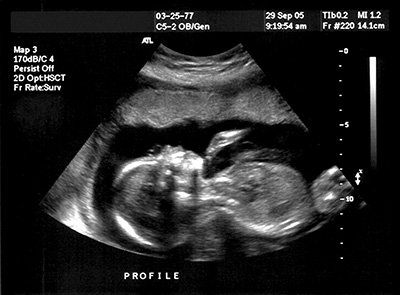
Demonstrated that whole-exome sequencing could serve as a valuable addition to standard prenatal genetic tests, with the potential to improve perinatal care for infants with genetic conditions
-
Developing a fetal cardiac intervention program for the treatment of certain cardiac anomalies in utero
-
Advancing predictive monitoring as an alternative approach to assessing hemodynamic status of infants in the NICU to optimize end-organ tissue oxygenation and decrease morbidity and mortality
-
Established The Mothers Center, which serves as a national model for providing comprehensive, multidisciplinary care for maternal complications before, during, and after a high-risk pregnancy with a single point of access to all of the subspecialists patients may need

-
First to implant a Berlin Heart as a bridge to transplant in the youngest patient ever to receive one – an infant only three days old

-
Established the only cardiac ICU in the nation exclusively dedicated to the care of newborn infants with congenital heart disease
-
Leaders in treating low-birthweight infants with early complicated conditions involving either a ventricular septal defect or aortic arch anomalies
-
Participated in a nationwide initiative to establish recommendations on reducing racial and ethnic disparities in maternal morbidity and mortality rates in the United States

-
Leader in New York State in efforts to reducing maternal morbidity and mortality, including New York State’s Safe Motherhood Initiative and Maternal Mortality Review Board
-
Implemented a Premature Care Bundle pilot project in Tanzania to increase survival of premature infants, achieving an overall 26 percent reduction in neonatal mortality

Outcomes
Neonatal Cardiac Surgery - Age <30 Days
In 2017, NewYork- Presbyterian’s survival rate after the Norwood procedure was 92%, which is among the best in the country.
Volume
2013 - 2017

Mortality
2013 - 2017

Source: Society of Thoracic Surgeons (STS) National Database 2017
Mortality Based on Complexity of Cases
2013 - 2017

Survival Following Arterial Switch Operation
2013 - 2017

Norwood Procedure Hospital Discharge Mortality
2013 - 2017