
Dr. Faisal Shaikh
Faisal Shaikh, MD, is Director of the Interventional Pulmonology Program in the Division of Pulmonary and Critical Care Medicine and the Thoracic Surgery Section at NewYork-Presbyterian/
Discovering a lung nodule can be a frightening and potentially protracted journey for patients, often taking months from discovery to diagnosis to treatment. With increasing computed tomography (CT) surveillance of the general population, we are finding more patients in the position of having an uncertain lung nodule. In more than 60% of the cases, the nodule is very small and sometimes in a location difficult to biopsy with traditional techniques. These patients may be relegated to serial observation with CT scans, which can be anxiety provoking.
When lung cancer in the nodule is suspected, the medical team will often require a biopsy either via a percutaneous, surgical, or bronchoscopic approach. A percutaneous transthoracic CT-guided needle biopsy involves a puncture through the pleural, a critical protective layering around the lung. Puncturing this membrane can result in complications which may necessitate a hospital stay or an ancillary procedure, such as insertion of a chest tube. Similarly, a surgical biopsy to excise the portion of lung with the nodule carries risks inherent to surgery and, according to national data, about 20 percent of these surgeries are ultimately found to have biopsied benign, non-cancerous nodules.
“The field of interventional pulmonology is much akin to interventional cardiology as it developed in the 1980s and interventional GI, which evolved in the 1990s,” says Dr. Shaikh. “Interventional pulmonology is born from exciting new technology that enables us to perform minimally invasive diagnostic procedures. With the advent of robotic bronchoscopy, we are now able to reliably and safely biopsy these potentially pre-cancerous lung lesions, even when in difficult to reach locations. The intention is to detect lung cancer at its earliest possible stage with the little or no risk to the patient. That is the state of care we can now offer our patients at NewYork-Presbyterian/
A New Paradigm of Care
NewYork-Presbyterian interventional pulmonology faculty are changing the paradigm of care for patients whose lung nodules are too small to biopsy until they are at a more advanced stage or for those who are potentially too ill to undergo a surgical or percutaneous biopsy.
“At NewYork-Presbyterian, about 30 percent of concerning lung nodules are identified through lung cancer screenings and, even more importantly, found incidentally on CT scans of the chest requested for other reasons, such as looking for a pulmonary embolus, pneumonia, or coronary assessments,” notes Dr. Shaikh. “We find about more than 8,000 nodules incidentally each year. Based on patient characteristics and features of the lung nodule, we identify nodules that are concerning and discuss what intervention is warranted. Reducing the time between discovery of the nodule and treatment is critical in the context of lung cancer. In certain cases, we see that lung cancer may grow from potentially a curable state to incurable within four to six weeks. If you can condense that time and minimize delays, you can significantly impact the lives of people.”
In July 2022, Dr. Shaikh introduced the latest technology for performing a lung biopsy at NewYork-Presbyterian/
With this minimally invasive approach, we are able to provide patients with an answer and reduce their anxiety of waiting for a potential cancer diagnosis that comes with the observational approach. This is an incredible relief for patients.
— Dr. Faisal Shaikh
“This changes the landscape of how we counsel a patient. We can now offer a minimally invasive procedure with virtually no complications as an alternative to surveillance monitoring or a surgical or percutaneous biopsy,” says Dr. Shaikh. “With this minimally invasive approach, we are able to provide patients with an answer and reduce their anxiety of waiting for a potential cancer diagnosis that comes with the observational approach. This is an incredible relief for patients.”
To date, Dr. Shaikh has performed approximately 180 cases at NewYork-Presbyterian/
Fundamentals of a Minimally Invasive Lung Biopsy
“The robotic software essentially allows us to map the procedure from start to finish,” explains Dr. Shaikh. “Based on the CT scan where the lung nodule was first identified, the nodule is recapitulated within the software to create a virtual 3D reconstruction that details the airways from the trachea through to the smaller bronchials. This gives you an incredible insight, and we are learning more about the human lung then we knew before. By enabling us to pinpoint the nodule in that 3D virtual space, we are able to size the nodule, look at its contour, and then navigate the robotic camera to meet the nodule from within without making any incisions.
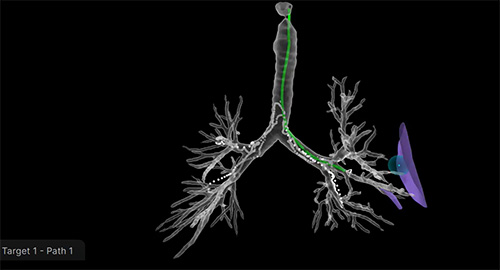
Real time 3D mapping is performed as the robotic arm is driving into 4 quadrants of the lungs. Following the generation of a 3D map, doctors can then drive the robotic arm with extreme accuracy to the nodule and perform biopsy.
“Once we have driven out to the nodule, we take an intraoperative low-dose radiation CT scan. From this, we can assess our relationship to the lung nodule and where to place the needle. Are we at the center of the nodule? Do we need to make minute adjustments to get the best tissue? With the robot and the CT scanner, we can now position the needle at the center of the nodule with incredible accuracy and incredibly fast. The average time of this procedure is 12-15 minutes from start to finish,” continues Dr. Shaikh.
Advancing from Diagnostic to Therapeutic Capabilities
As studies continue to support interventional pulmonology as a valid and reliable method comparable, for example, to interventional cardiology, the goal would be to progress from using the approach to establish a diagnosis to being able to perform a curative procedure. “This technology has the potential for delivering treatment, whether a radiofrequency ablation, radiation therapy from within, or a pharmaceutical approach in which sensitizing agents or chemotherapy can be injected directly into tumors,” says Dr. Shaikh. “This would be particularly significant for patients who need treatment but who are not candidates for surgery due to comorbidities, age, frailty, or prior lung surgeries. An endoscopic radiofrequency ablation may not necessarily replace current forms of treatment, but rather become another tool that expands the options for patient care.”




