A recent study led by Jason D. Wright, M.D., chief of the division of gynecologic oncology at NewYork-Presbyterian and Columbia, projects a significant increase in both the incidence and mortality of uterine cancer in the U.S. over the next three decades. The forecast for uterine cancer rates among Black women is particularly alarming, with mortality projected to be about two-and-a-half times higher than that of white women. The study’s results were published in Cancer Epidemiology, Biomarkers & Prevention.
“Prior studies have consistently shown significant racial disparities among Black and white women with uterine cancer,” says Dr. Wright. “Our study further illustrates the substantial burden this cancer places on Black women, who are more frequently diagnosed with aggressive forms of uterine cancer, often face delayed diagnosis that results in later-stage disease, and who experience delays in treatment.”
Our study further illustrates the substantial burden this cancer places on Black women, who are more frequently diagnosed with aggressive forms of uterine cancer, often face delayed diagnosis that results in later-stage disease, and who experience delays in treatment.
— Dr. Jason Wright
Modeling the Trajectory of Uterine Cancer
As part of the National Cancer Institute’s (NCI) Cancer Intervention and Surveillance Modeling Network (CISNET), Dr. Wright and his colleagues created the Columbia University Uterine Cancer Model (UTMO), a natural history model based on population data designed to simulate U.S. uterine cancer trends through 2050. “We utilized data from various sources, including cancer registries, national health surveys, and epidemiological studies, to understand the trajectory of women with uterine cancer in this country,” says Dr. Wright. “Once we developed the baseline model, we projected future incidence and mortality rates for uterine cancer.”
The model simulates the experiences of non-Hispanic white and non-Hispanic Black women separately, starting at age 18 and continuing until age 84, across four general states: healthy; precursor lesion, or endometrial intraepithelial neoplasia; uterine cancer; and death. It also considers different tumor histologies (endometrioid versus non-endometrioid) and factors such as hysterectomy rates to predict future outcomes. “We know that if a patient has had a hysterectomy, they’re no longer at risk for uterine cancer,” says Dr. Wright. “However, hysterectomy rates have been declining in the United States, which is an important factor in projecting uterine cancer rates.”
Rising rates of obesity were also factored into the projections. “Adipose tissue produces estrogen, which stimulates the growth of the endometrium,” he adds. “This makes obesity one of the strongest risk factors for uterine cancer.”
UTMO was calibrated and validated against historical data from the NCI’s Surveillance, Epidemiology and End Results (SEER) cancer registry, demonstrating a close alignment with observed incidence and mortality rates through 2018.
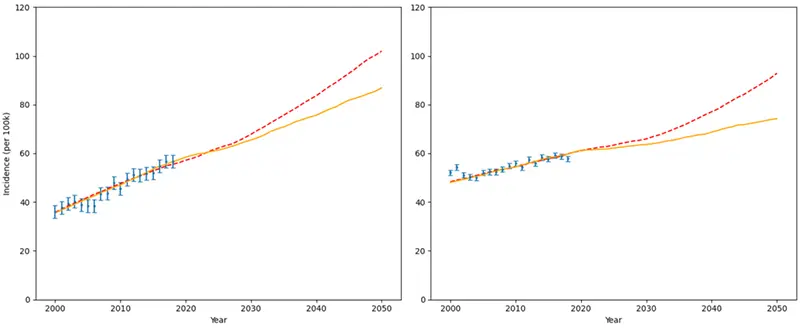
UTMO incidence projections per 100,000 people for non-Hispanic Black women (left) versus white women (right). The red dotted-line trajectory incorporates projected changes in obesity and hysterectomy rates; the yellow line trajectory reflects no changes in obesity and hysterectomy rates. The blue symbols reflect SEER data. Chart courtesy of Columbia.
Disparities Will Continue to Grow
The study’s projections indicate a continued rise of uterine cancer rates even if hysterectomy and obesity rates don’t change, highlighting how racial disparities are expected to widen. Specifically, the research team estimates that:
- The incidence rate for Black women is projected to rise to 86.9 cases per 100,000 by 2050, a 53% increase from 56.8 in 2018. The incidence for white women will increase to 74.2 cases per 100,000, a 29% increase from 57.7 in 2018.
- The incidence-based mortality rate for Black women will nearly double from 14.1 to 27.9 per 100,000; it will also increase for white women from 6.1 to 11.2 per 100,000.
A key biological driver of the widening mortality gap is the disproportionate increase in aggressive, non-endometrial uterine cancers among Black women. The research estimates that the incidence of these cancers will rise from 22.5 to 36.3 cases per 100,000 for Black women, but only from 8.5 to 10.8 cases for white women. Additionally, the malignancy sojourn time — the asymptomatic period when a cancer is screen-detectable — is significantly shorter for non-endometrial cancers (about eight months) compared to endometrial cancers (about 22 months).
“The non-endometrioid cancers tend to be more aggressive and progress from early to advanced disease more quickly,” says Dr. Wright. “They are also more common among Black women, contributing to the disparities in care. Unfortunately, we have a shorter window for patients to present with symptoms, limiting our ability to intervene and improve overall survival.”
The Need for Better Uterine Cancer Treatment and Detection
While the model’s results are sobering, the research can help inform future cancer prevention efforts. “This paper shows that there is a significant window for early detection of uterine cancer,” says Dr. Wright. “That’s why we’re part of a larger multidisciplinary project testing novel approaches to screening and prevention aimed at reducing the disease burden for women.”
One factor not accounted for in the model is new breakthroughs in uterine cancer treatments. “We now have a better understanding of the molecular biology and genetics of the disease, which has led to improved therapies like immunotherapy, now more commonly used for patients with advanced or metastatic disease,” he says. “A future direction of our work is to integrate some of these new treatments into the model to assess their potential impact on mortality.”
Ultimately, the study provides further evidence of the need for better understanding and treatment of uterine cancer, and further research is being planned that will include other racial groups and additional risk factors. “Uterine cancer is often a type of cancer that we don’t think about enough,” says Dr. Wright. “However, we need greater recognition of its symptoms by both physicians and patients, as well as higher quality, more timely evaluations to move the needle. These results will help inform the development of robust strategies and new therapies aimed at reducing the burden and enhancing patient outcomes.”




