For patients with complex spinal deformities, traditional open surgical approaches have meant large incisions and extended recovery periods. While advancements in anterior and posterior minimally invasive spine surgery (MISS) have helped improve the patient experience, accommodating the size of implants and intraoperative patient repositioning still pose limitations.
At Och Spine at NewYork-Presbyterian and Columbia, neurological spine surgeons Andrew Chan, M.D., director of minimally invasive scoliosis surgery, and Dean Chou, M.D., chief of the Spine Division, are using advanced lateral access and single-position surgical techniques to overcome these hurdles, enhancing surgical efficiency and improving patient outcomes. “Our goal is to provide the most effective and least invasive treatment possible to our patients to help them return to their lives with less pain and improved function,” says Dr. Chou. “These approaches are the future of MISS and will continue to move the field forward.”
How a Lateral Approach Overcomes Traditional Surgical Limitations
Surgical repair for spinal deformities often necessitates fusion, a procedure that requires screws, rods, and interbody cages for stabilization. However, with a posterior approach, “we are limited in the size of the cage we can implant due to the various nerves in our way," explains Dr. Chan.
The alternative, a traditional anterior approach, requires a large incision from sternum to pelvis and mobilization of the abdominal organs, which increases morbidity. “While anterior and posterior approaches work, it’s like taking the long road with many detours to reach the final destination,” Dr. Chou adds.
Our goal is to provide the most effective and least invasive treatment possible to our patients to help them return to their lives with less pain and improved function.
— Dr. Dean Chou
Dr. Chan and Dr. Chou are now approaching spine surgery laterally using lateral transpsoas and antepsoas (ATP) approaches to avoid dissecting the muscles and nerves in the back and permit the implantation of larger interbody cages to provide greater stabilization. Both MISS approaches offer a more direct pathway to the spine via a one-inch incision through the side of the body, using imaging as a guide.
"Because we avoid the posterior muscles and nerves, we are able to insert a much larger cage, restore the height of intervertebral discs, and achieve indirect decompression of the spine at single or multiple levels," says Dr. Chan. “The clinical benefits are substantial, including shorter recovery times, less blood loss, and superior spinal alignment.”
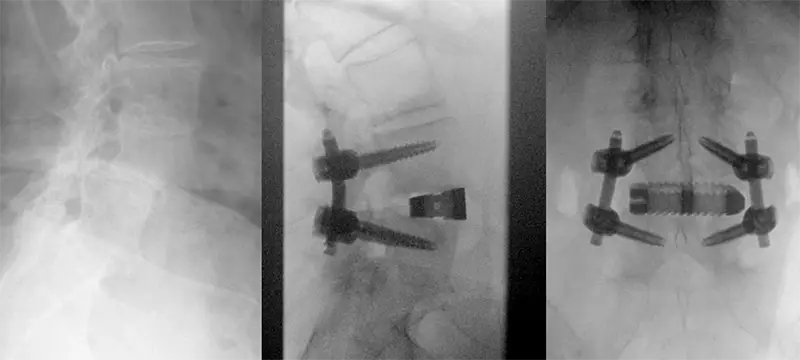
A case of L4-L5 spondylolisthesis treated with the prone lateral approach, resulting in completed restoration of disc height and reduction of the slip.
ATP and transpsoas approaches are applicable for many pathologies of the thoracic and lumbar spine, including scoliosis, spondylosis, spondylolisthesis, degenerative disc disease, stenosis, and disc herniations; however, patients with conditions of the cervical spine do not qualify for a lateral approach.
The Added Advantages of Single-Position Surgery
Building on the advantages of the lateral technique, single-position surgery addresses the other major inefficiency of staged procedures: patient repositioning. Historically, even a lateral approach was often followed by a “flip” to the prone position for posterior instrumentation if screws and rods were necessary for stabilization. “This flipping of the patient adds significant time to the surgery, increases time under anesthesia, and requires a second sterile setup,” Dr. Chou notes.
By using specialized operating tables and imaging equipment, surgeons can now perform both the lateral and posterior portions of the procedure without moving the patient. "With single position surgery, we can perform both parts of the procedure — placing the cage from the side and the screws from the back — while the patient remains only in the lateral or prone position,” says Dr. Chan. “This makes the entire operation more efficient, decreases anesthesia exposure to the patient, and enables us to keep the support structure of the spine as stable as possible.”

Dr. Chan performing lateral surgery via a one-inch incision on a patient in the prone position.
The impact of avoiding patient repositioning is profound. “The primary benefit is a dramatic reduction in operating time,” Dr. Chan says. “We can shave an hour or more off a procedure.” Less time in surgery translates directly to improved patient outcomes, including:
- Faster recovery and quicker mobilization
- Lower risk of complications associated with prolonged anesthesia
- Decreased blood loss
- Shorter hospital stays
This streamlined protocol marks a paradigm shift, which the experts at Och Spine at NewYork-Presbyterian and Columbia already have the experience to perform. “It represents a major leap forward in our ability to treat complex spinal disorders in the least invasive way possible,” says Dr. Chan.





