A mammogram can reveal whether a woman has dense breast tissue, a feature linked to a higher risk of breast cancer that requires extra screening. However, findings from a new study published in Radiology suggest that six different breast texture patterns, which can also be seen on mammograms, do a better job of predicting breast cancer than breast density.
A computer algorithm developed by Columbia and Mayo Clinic researchers that detects and quantifies the patterns could soon be added to digital mammography systems to provide clinicians with better risk estimates.
“These tools will pave the way for personalized screening recommendations and better management of women’s health care, reducing the frequency of screening for low-risk women and increasing the frequency for women who need it,” says study co-leader Despina Kontos, Ph.D., professor of radiological sciences and vice chair of artificial intelligence and data science research in the Department of Radiology at Columbia. “They may also help us do a better job of identifying women who would benefit from interventions to lower their risk of breast cancer.”
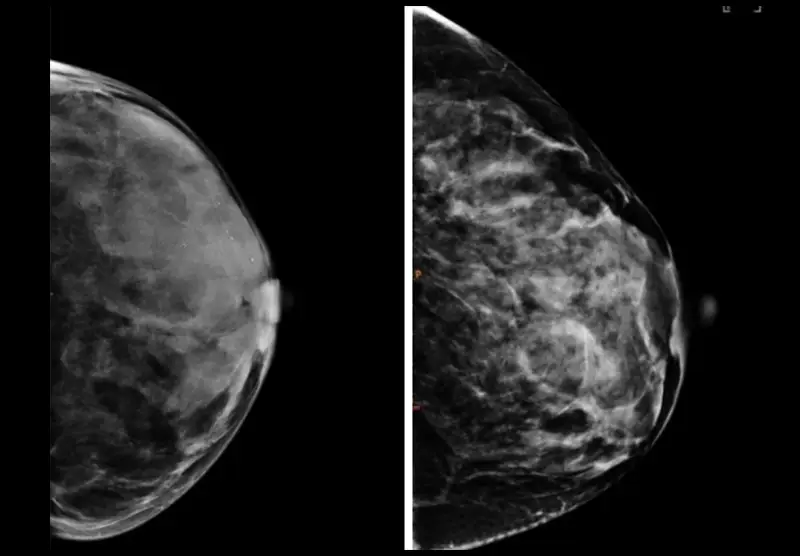
Breasts with the same density can have vastly different breast textures, as seen in the mammography above. Images courtesy of Despina Kontos/Columbia.
Unlocking More Information From Mammograms
Since the adoption of digital mammography about two decades ago, computer scientists like Dr. Kontos have been looking to capture details from mammograms that go beyond breast density and better predict individual risk.
Smaller, earlier studies suggested that differences in texture — patterns in the way fat and glandular tissue is distributed in the breast — may also be related to breast cancer risk.
“Different patterns are visible to radiologists who examine mammography images — some look clumpy, some look smooth, some look more spotty,” Dr. Kontos says. “But beyond making a determination of overall density, radiologists had no way to quantify these patterns and turn them into data needed to determine their link to cancer risk.”
The new study, one of the largest of its kind, featured a two-stage design:
- The first stage was a retrospective cross-sectional analysis of four-view, full-field digital mammography images from 30,000 randomly selected women, which used radiomics to identify different parenchymal phenotypes (breast texture patterns).
- The second stage was a nested case-control study examining those phenotypes on the mammograms of 1,055 women with invasive breast cancer matched to 2,764 women without breast cancer.
Screening is the cornerstone of early detection. Improving its ability to make predictions will increase its role in breast cancer prevention.
— Dr. Despina Kontos
The researchers’ analysis showed that six phenotypes that measure the complexity of the breast tissue were found to be associated with greater breast cancer risk in both white and Black women. The patterns were also positively associated with false negative findings and symptomatic interval cancers.
“Given that women with the same breast density can have substantially different texture patterns, our analysis provides important additional information for estimating breast cancer risk,” Dr. Kontos says.
Additional data, including genetics and lifestyle information, are being included in the computer algorithm to see if its predictive power can be increased further. Dr. Kontos and her collaborators are also experimenting with AI approaches that may reveal predictors currently hidden in the mammography data and extending their analysis to 3D mammography images.
“Screening is the cornerstone of early detection,” Dr. Kontos says. “Improving its ability to make predictions will increase its role in breast cancer prevention even further.”
A version of this article originally ran on the Columbia newsroom.




