For more than two decades, nipple-sparing mastectomies have provided breast cancer patients with a surgical option that removes breast tissue while keeping the skin, nipple, and areola intact, with the goal of providing a more natural appearance after breast reconstruction. While the procedure provides better aesthetics over traditional or skin-sparing mastectomies, scarring is still visible where the incision is made underneath the breast.
An evolution of the procedure known as the endoscopic nipple-sparing mastectomy (E-NSM) minimizes scarring even further, providing better cosmetic results using minimally invasive techniques, smaller incisions, and different incision placement. The novel procedure has been performed in Europe and Asia for several years but was only introduced to the United States in 2025. NewYork-Presbyterian and Weill Cornell Medicine breast surgical oncologists Vivian Bea, M.D., and Olivia Cheng, M.D., were among the first to perform E-NSM in the U.S.
“We can decrease the incision to 3 centimeters, which helps with cosmesis,” says Dr. Bea, who is section chief of breast surgical oncology at NewYork-Presbyterian Brooklyn Methodist. Using laparoscopic techniques, “we’re also able to insufflate the breast space in a way where we can really see the breast parenchyma. Nipple-sparing mastectomies can be one of the more challenging procedures because of the small space we work in, but being able to do them endoscopically provides better visualization.”
How E-NSM Differs From Conventional Nipple-Sparing Mastectomies
Open nipple-sparing mastectomies typically require about a 5-to-7-centimeter incision in a half-moon shape along the inframammary fold. With E-NSM, an incision of approximately 3 centimeters is made on the side of the breast along the anterior or mid axillary line, in line with the nipple-areola complex. This placement not only makes the post-surgical scar less obvious, it also provides surgeons with access to the sentinel lymph node for biopsy, if necessary, without requiring a second incision.
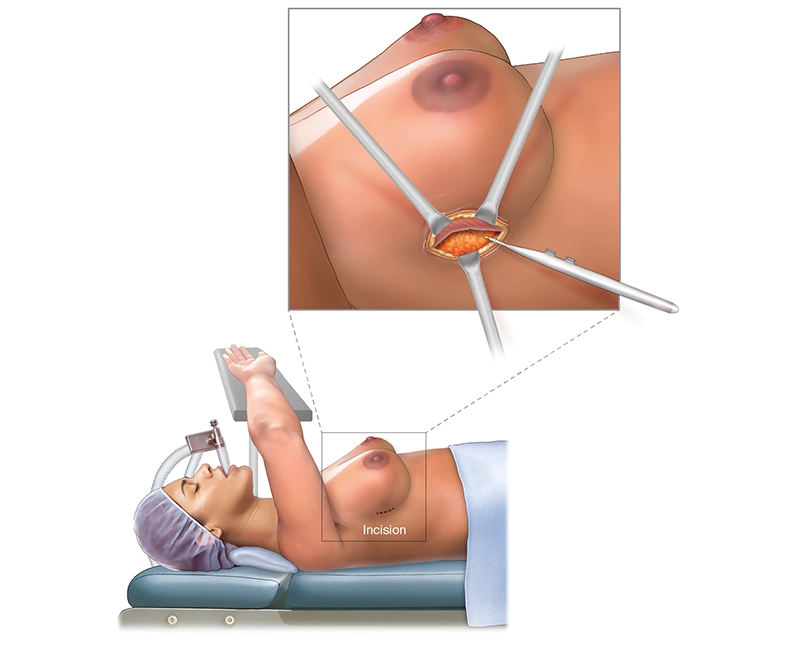
In an endoscopic nipple-sparing mastectomy, an approximately 3-centimeter incision is placed along the side of the breast. The arm can be supported either overheard, as pictured, or below the table.
Surgeons can typically perform about half of the dissection through the incision with direct visualization before switching to endoscopic dissection, when a port assist device is inserted to hold the endoscope and laparoscopic instruments in place; insufflation is also used to improve visibility. “E-NSM allows for better ergonomics for the surgeon. Another advantage is that residents and medical students are able to visualize the breast parenchyma, which leads to better teaching opportunities,” says Dr. Bea.
Once the breast dissection is complete, a special funnel can be used to help insert the breast implant through the incision for reconstruction. As with an open procedure, patients may be discharged on the same day or stay one night, spend two to three weeks with a drain, and resume normal activities shortly thereafter. However, unlike with traditional NSMs, they are left with just a barely perceptible 3-centimeter scar.
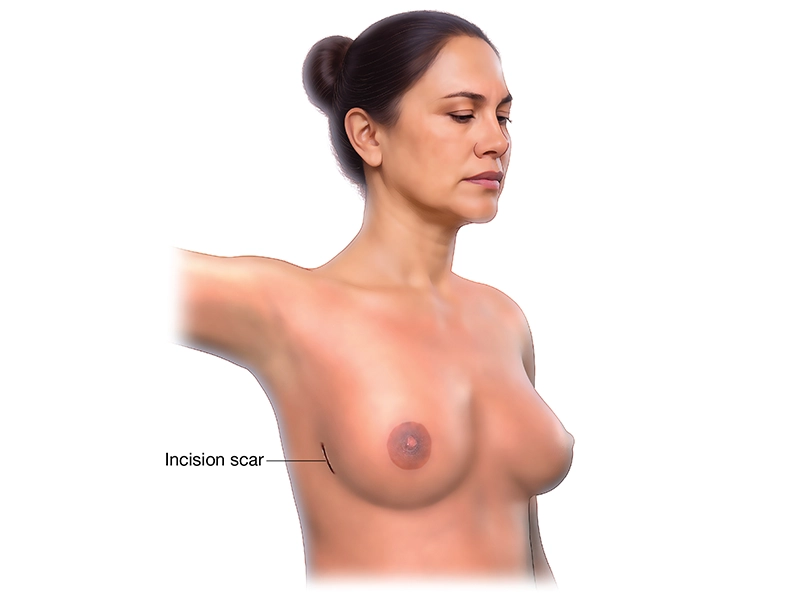
Post surgery, the patient is left with an approximately 3-centimeter scar.
International studies have shown that oncological outcomes of E-NSM were not inferior to conventional nipple-sparing mastectomies and, while more research needs to be done, some early data indicates potential benefits beyond aesthetics. “The advantage is really the cosmetic benefit for patients, but there are early reports that there could be advantages for nipple sensation and skin integrity,” explains Dr. Bea.
Pioneering E-NSM in the U.S.
As a specialist in skin-sparing and nipple-sparing mastectomies and oncoplastic breast conservation surgery, Dr. Bea was in the early wave of U.S. breast surgeons to receive E-NSM training, traveling to Amsterdam in April 2025 to learn the procedure from European surgeons; Dr. Cheng received training in the U.S. a few months later. After identifying a suitable candidate at NewYork-Presbyterian Brooklyn Methodist who was to undergo a double mastectomy, their team performed one of the first endoscopic nipple-sparing mastectomies in the country in June 2025. “After learning about E-NSM, I realized it was possible to perform the procedure through an even smaller incision than what we’re used to,” says Dr. Cheng. “It takes the surgery to the next level.”
As with conventional NSMs, E-NSM is not suitable for all breast cancer patients. The best candidates are those whose cancers are away from the nipple or skin, and who have small breasts with no ptosis. “There’s a higher risk of ischemia if the cancer is very close to the nipple, and if the breasts are too large or the patient has ptosis, there’s a higher risk of poor wound healing,” explains Dr. Cheng.
Close collaboration with a plastic surgeon who can adapt their reconstruction techniques is also key for E-NSM. Finding suitable arm positioning with the appropriate level of padding to minimize neuropraxia for patients may also take some trial and error, and the newness of the procedure means it may take longer to perform.
As E-NSM becomes more common and as more data is collected, Drs. Bea and Cheng believe surgical times will get shorter, and E-NSM could become a new standard of care for patients who qualify. They are now training other surgeons on the procedure, including a recent session in a simulation lab at Columbia. “All breast surgeons have had laparoscopic training through general surgery residency, but laparoscopic procedures haven’t been as common in breast surgery as in other specialties,” says Dr. Bea. “This makes for a unique opportunity to incorporate previously learned skills for minimally invasive breast surgery.”
“We’re still in the early days of learning about the benefits of the endoscopic approach,” adds Dr. Cheng. “As more cases are performed in the U.S., yielding more patient information and more surgeons who are comfortable with the procedure, we can really start to explore the benefits beyond cosmesis.”