In late October 2023, a pregnant woman presented to the emergency room at NewYork-Presbyterian/
Below, her NewYork-Presbyterian/
How did the patient present when she arrived at the emergency room?
She presented to the emergency room with leg pain and some edema. She received a lower extremity venous ultrasound which showed an iliofemoral DVT. When a DVT occurs in pregnancy, it is imperative to address it as quickly as possible. She was immediately transferred to the maternal-fetal medicine service, where we admitted her, examined her right away and started her on a heparin drip.
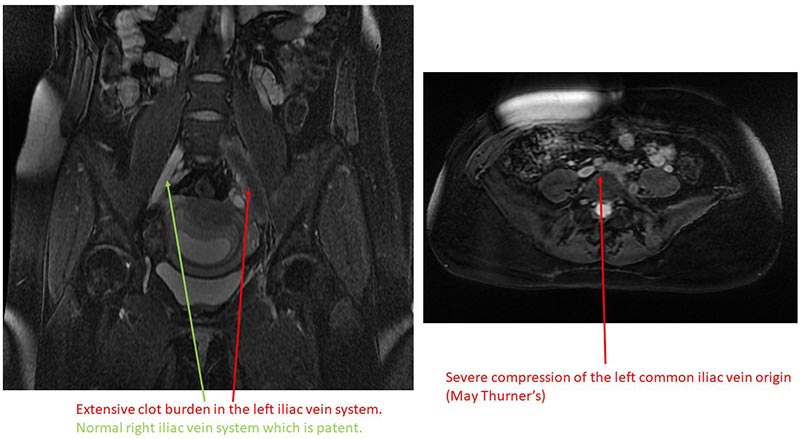
Extensive clot burden in the left iliac vein system and severe compression of the left common vein origin.
How common is it for a pregnant woman to develop a DVT?
Pregnancy increases the risk for a blood clot five-fold. When we performed the imaging, we discovered that she had May-Thurner Syndrome. Her right iliac artery was compressing the left iliac vein. Several patients with May-Thurner Syndrome typically experience no symptoms and remain undiagnosed, yet some develop DVT like our patient did.
What was her prognosis after starting heparin?
While heparin does not break up blood clots, it is helpful in preventing clot propagation and the formation of new clots. Unfortunately, after being hospitalized and despite being on therapeutic anticoagulation for 48 hours, she started getting worse. Her leg was much more swollen, and it started to become bluish in color. The symptoms were unbearable that she couldn’t stand on that leg. A multidisciplinary meeting was held with maternal fetal medicine and the CLOT team, which is a multidisciplinary team which treats patients with complex DVTs and includes hematology and interventional radiology clinical services. Although it might be common to have a patient with DVT, the fact that she was pregnant and did not respond to conservative management increased her risk exponentially. At that point, Interventional Radiology began considering endovascular, minimally invasive treatment options to remove her clot.
Right iliac artery compressing the left iliac vein
What were her treatment options after conservative management failed?
The published guidelines for management of thrombotic events during pregnancy include the use of heparin or enoxaparin (a low molecular weight heparin), which she did not respond to. There are no published evidence or guidelines for managing such a complicated DVT in pregnancy if medical therapy fails. So we rapidly convened a multidisciplinary team including maternal-fetal medicine, hematology, and interventional radiology in order to discuss her options, weigh the risks and benefits of each option as well as decide what the best approach would be.
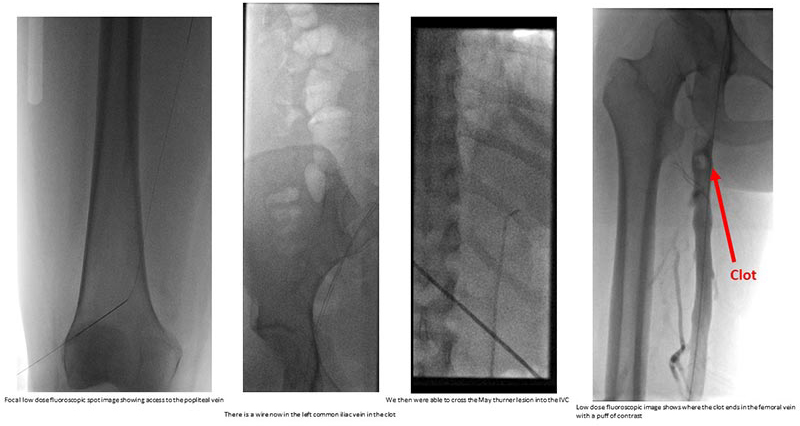
Ultimately, we decided the appropriate course of treatment would be adjunctive endovascular intervention, called mechanical suction thrombectomy. The clot she had was substantial. We were especially worried that if this clot were to be dislodged and sent to the heart, it would risk cardiopulmonary compromise and cause the heart to stop beating. In the past, these procedures required tPA (tissue plasminogen activator), a drug which can dissolve blood clots, but can cause severe uncorrectable bleeding. Recent advances in technology, offered at NewYork-Presbyterian, have allowed for a much safer way to debulk this clot and can be performed safely and minimally invasively. We were concerned about the use of radiation that this procedure requires, especially in this pregnant patient in her first trimester, but we were able to use additional tools to minimize that risk.
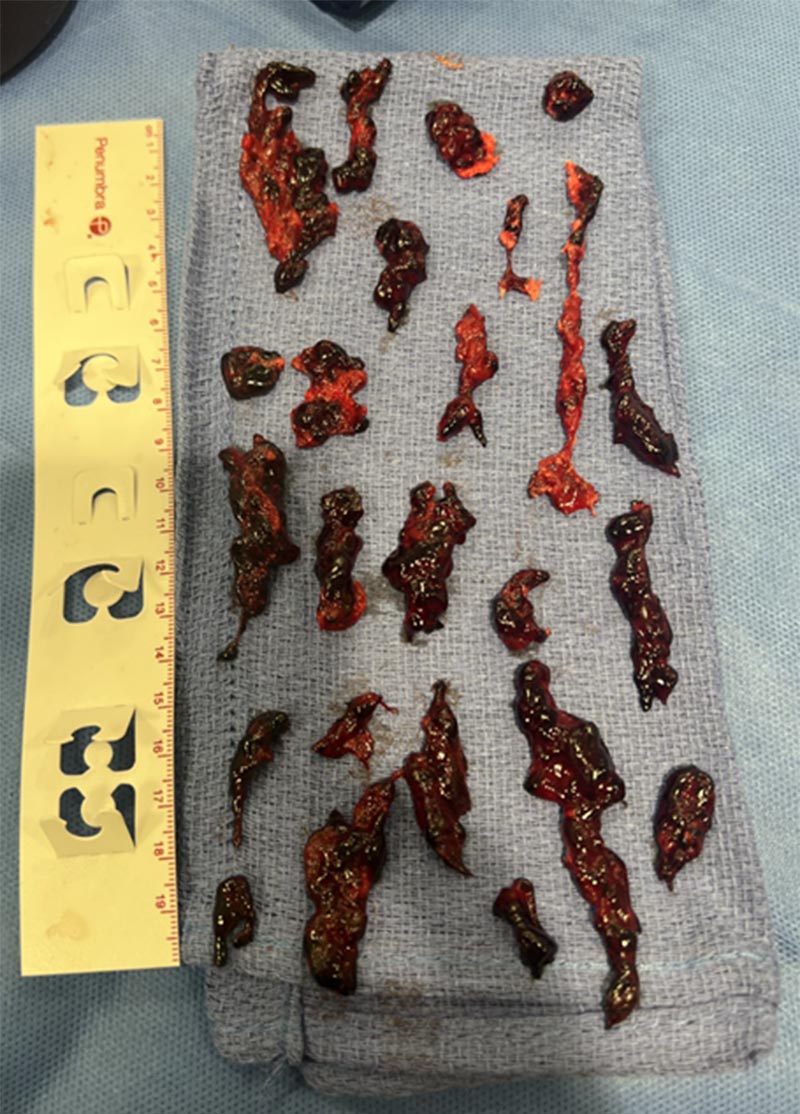
Remnants of the blood clot after the mechanical thrombectomy
We performed a low-dose diagnostic venography and intravascular ultrasound which demonstrated an occlusive thrombus extending throughout the left common iliac vein, left external iliac vein, and left common femoral vein. We accessed the popliteal vein in the back of her knee and used a large bore catheter to debulk the clot from the knee (peripheral) to the lower abdomen (central). We successfully evacuated the clot with minimal residual clot burden seen on post-thrombectomy venography and intravascular ultrasound. Total radiation to the patient and fetus was less than 2 plain film X-rays.
How is she doing now?
The patient went to the ICU overnight for close monitoring following the procedure. Clinically, she did fantastic. The following morning her leg swelling had markedly improved and her pain had resolved. She was able to walk 100 feet without pain and she was discharged home in the afternoon directly from the ICU. In follow up since then, her leg swelling is completely resolved, and she is focused on getting back to living her life. It was extremely gratifying was for us to play a part in her recovery and watch her go from being debilitated and bed bound to almost normal the next day.
When she arrived at the emergency room, she was not a patient at NewYork-Presbyterian. She has since switched her care to being followed by NewYork-Presbyterian/Columbia physicians in maternal-fetal medicine, hematology, and interventional radiology. She will need to remain on anticoagulation throughout the rest of her pregnancy and a few weeks after in order to minimize the risk of a recurrent clot. She will keep an eye out for warning signs and remains in close contact with our team.
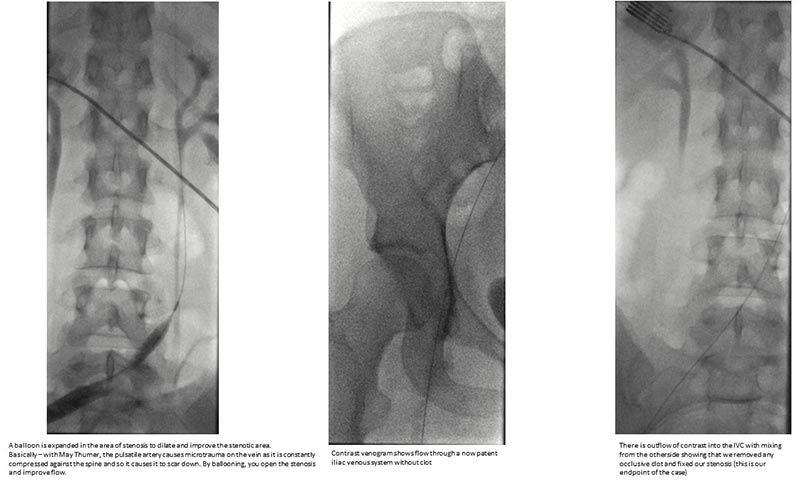
Successful clot evacuation with minimal residual clot burden seen on post-thrombectomy venography and intravascular ultrasound
What did you take away from this case?
If providers have a pregnant patient with extensive DVT, they should not be afraid of advanced interventions such as endovascular thrombectomy due to potential exposure to radiation. We took precautions to focus the radiation below the pelvis to limit radiation risk to the baby. In the end, our patient was exposed to as much radiation as two plain film x-rays, which is insignificant.
Importantly, treating DVT in pregnancy requires a multidisciplinary approach, and it is not something that every hospital is equipped to handle. At Columbia, we have a CLOT team which is a unique collaboration between Interventional Radiology and Hematology to treat patients who have complex DVTs. Because our departments work so closely every day, we were able to have OB and our CLOT team work closely, discuss the case, and quickly reach a consensus on the best approach to treat this patient. We are glad that she is feeling better and back on her feet.







