In 2019, the Food and Drug Administration approved anterior vertebral body tethering for patients with adolescent and idiopathic scoliosis who have growth remaining as an alternative to the standard treatment – posterior spinal fusion and instrumentation. In the tethering procedure, vertebral body screws and a flexible tether are placed laterally from a thoracoscopic or thoracotomy approach into the vertebral body on the convex side of a spinal deformity. A tensioning cord is secured to the vertebral body screws with set screws to connect the levels of the construct. The device provides a lateral tension band across the convex side of the spine that, on insertion and tensioning, partially corrects the curvature, and subsequently can arrest or correct the deformity through modulation of remaining spinal growth.

Dr. Michael Vitale
“I have been heavily involved with the development of tethering and have also been involved with clinical research of this procedure,” says Michael G. Vitale, MD, MPH, Chief of Pediatric Spine and Scoliosis Surgery in the Department of Orthopedic Surgery at NewYork-Presbyterian/Columbia University Irving Medical Center and the Ana Lucia Professor of Pediatric Orthopedic Surgery and Neurosurgery at Columbia. “It has been gratifying to watch this develop and also to understand the true outcomes and potential of this growth modulating, non-fusion technique.”
Dr. Vitale guides patients and their parents through the decision-making process as to which approach might be appropriate in correcting their curvature. “Both of these techniques have advantages and disadvantages,” says Dr. Vitale, who specializes in the non-operative and operative treatment of complex pediatric scoliosis, kyphosis, and adolescent Idiopathic scoliosis, performing some 200 scoliosis procedures every year. “I see my role not as a medical dictator, but as an aggregator of information for the families. Many of my patients are coming to me for a second opinion. Many are quite medically literate, and I get to act as a filter for the available information to these patients.”
Thoracic Tether vs. Fusion: Criteria and Outcomes
| Vertebral Body Tethering | Spinal Fusion |
|---|---|
| Curve: 40 to 60 degrees | Curve: >50 degrees |
| Flexible curves | Flexible or inflexible curves |
| Compensatory curve less than 45 degrees | Any size compensatory curve |
| Mild amount of rotation | Mild to severe rotation |
Skeletally immature
| Skeletally immature or mature
|
| Minimally invasive thorascopic surgery | Open surgery through a 20 cm incision |
| Length of hospital stay: 2 days | Length of hospital stay: 3 to 4 days |
| 10 to 15 percent risk of reoperation | 1 to 2 percent risk of reoperation |
| Little to no loss of flexibility | Possible loss of flexibility depending on the lowest level fused |
| Return to sports at 6 weeks | Return to sports at 6 weeks |
Through leadership efforts with the Pediatric Orthopedic Society of North America, the Pediatric Spine Foundation and Pediatric Spine Study Group, Dr. Vitale leads advocacy efforts with the FDA to improve access to pediatric devices and is specifically interested in innovative treatments that improve the quality and safety of patient outcomes. “The Pediatric Spine Study Group is a national registry of some 10,000 patients with scoliosis, and of this number, almost 500 patients have undergone tethering,” he says. “My close involvement with the PSSG and with research, which is constantly emerging at national meetings, enables me to update my patients with the latest information.”
While Dr. Vitale personally performs 10 spinal fusions for every tethering approach, he explains the pros and cons of both procedures. “I think the reliability of the spinal fusion is much higher. In other words, about 15 percent of the time tethering does not work as well as we would like and the patient needs another operation, usually a fusion,” he says. “The possibility of having to perform another operation after a fusion is very, very low, perhaps 1 to 2 percent. So, that is an important piece of data that goes into decision-making. The flip side is that tethering provides the opportunity to preserve more flexibility and motion, predominantly in the lumbar spine, as compared to the fusion.”
According to Dr. Vitale, patients who are very athletic – for example, dancers and gymnasts – may opt for tethering, especially in patients who would otherwise need a lumbar spine fusion. “In some situations, it might be worth the 15 percent chance of needing another operation. That’s what the decision comes down to,” he says. “In my practice, patients generally choose the tether on the order of 7 or 8 percent of the time.”
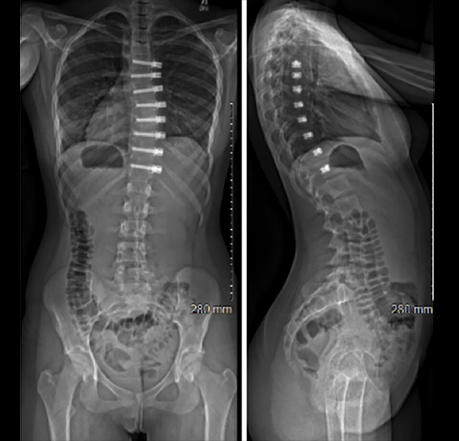
A) Tethering
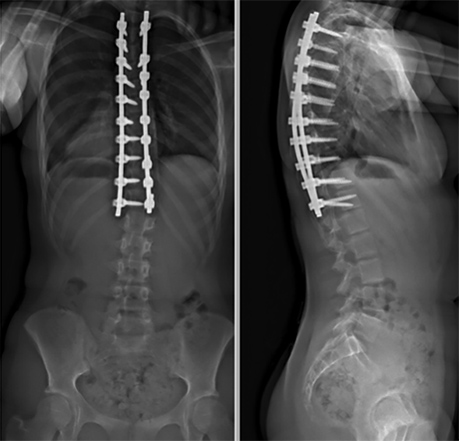
B) Fusion
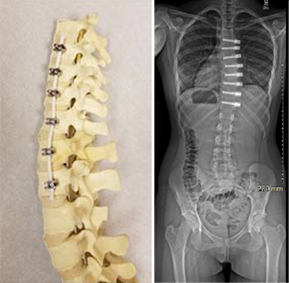
(Left) VTB hardware and postop X-ray
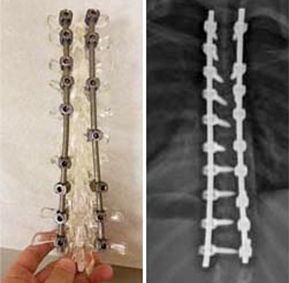
(Right) Fusion hardware and postop X-ray
Tethering is appropriate for only a subset of patients based largely on skeletal maturity, notes Dr. Vitale. “While some surgeons are only performing tethering, this is still a new technology with unknown long-term outcomes. The decision between fusion and vertebral body tethering is still evolving and is a case-by-case discussion and decision between the surgeon, patient, and the family.”
“I feel that the tether does need to be an option for some patients,” continues Dr. Vitale. “As a case in point, some years ago one of my patients had a traditional fusion surgery. Then her sister developed scoliosis and opted for a tether. They have both done very well. For surgeons like myself whose practice is 100 percent in pediatric scoliosis, I believe we need to have it in our armamentarium as an offering to patients with appropriate indications and transparency about all aspects of this approach.”




