Craniosynostosis occurs in one out of 2,000 live births. Caused when the individual bones of the skull fuse too early, the condition requires a technically demanding surgery to correct the anatomical abnormalities. Caitlin Hoffman, MD, is a pediatric neurosurgeon with NewYork-Presbyterian/

Dr. Thomas Imahiyerobo and Dr. Caitlin Hoffman
“This is a very unique aspect of our institution in that children that fall in the surgical category, as well as those with non-surgical disorders such as plagiocephaly, often have involvement of many additional systems that need to be addressed simultaneously,” says Dr. Hoffman. “Our program takes the onus off of the family and the primary care practitioner to coordinate all of that very complex care. The clinic is housed in one place that allows patients and their families to have their appointments in a centralized location, where 10 or so different subspecialists come to them and decisions about care plans are made in a collaborative way. This teamwork builds momentum that pushes and drives programmatic growth.”
Complexities of Craniosynostosis
According to Dr. Hoffman, unlike plagiocephaly, which can be managed non-surgically, craniosynostosis requires surgical modification not only to create a cosmetically desirable result, but more importantly, to optimize functional outcomes and cognitive development.
“An infant skull is composed of multiple tectonic plates that are open to allow for both overriding and adjustment during delivery, but also for accommodation of brain growth after delivery,” says Dr. Hoffman, a national leader in craniofacial surgery. “The plates are joined by flexible bands called sutures that allow the skull to adjust for rapid brain growth. When the brain reaches its full size, the sutures harden and the plates fuse. If one or more of those sutures hardens too early, the brain then looks for alternate areas to grow using the remaining open sutures. This results in craniosynostosis and its characteristic head shapes and the potential for neurocognitive deficits.”
The goal of surgery is threefold: to restore a normal trajectory for brain growth; to provide an environment for normal intracranial pressure; and to improve the morphology of a child's head, eye, and ear growth for a better cosmetic outcome. By removing the fused suture, the process of compensation can be arrested, allowing for correction towards normal dimensions and directions of calvarial growth over time and improvement of the overall visual appearance of the child.
The Value of Virtual Surgical Planning and 3D Imaging
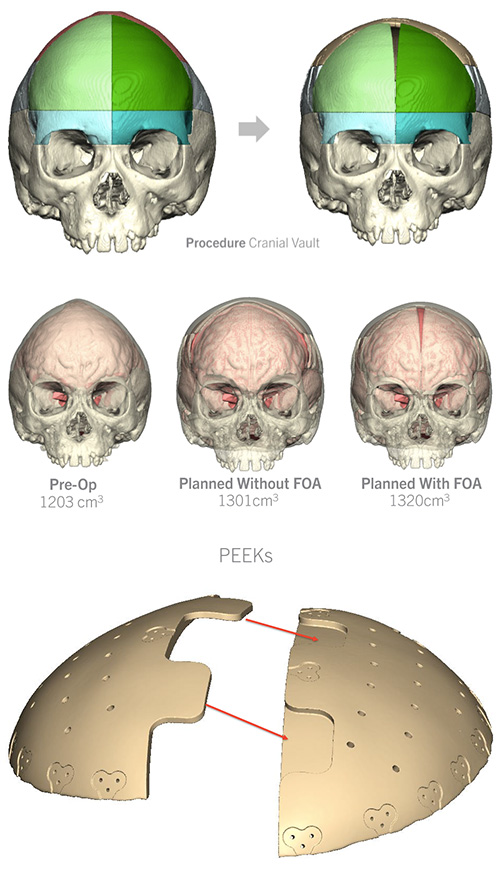
Historically, the success of craniofacial surgery, with the exception of a few rudimentary measurements, has been based on the surgeon’s assessment of room for brain growth and improved aesthetic appearance. To address this shortcoming, Dr. Hoffman and her colleagues are now using virtual surgical planning to create a surgical flight plan that can be modified virtually, providing the surgeons with an exact plan to follow on the operating table. The virtual planning also has helped to create a more collaborative approach with families.
“We want to move the needle forward to bring craniofacial surgery into a much more objective and scientific domain to aid in determining when children have achieved their most optimal corrections,” says Dr. Hoffman. “Instead of leaving it up to the surgeon to say, ‘It looks OK,’ we examined how we could preemptively improve patient outcomes and create a system of metrics to determine outcomes.”
The pediatric neurosurgical team at NewYork-Presbyterian/Weill Cornell Medical Center is assisted in their efforts by the availability of 3D technology combined with preoperative data on a patient’s presentation, intraoperative factors of how much bone was able to be removed, and the rate at which patients begin to correct postoperatively. They are now planning a study to evaluate this approach to better define outcomes, surgical successes, and the need for surgical revisions.
Virtual Surgical Planning for Cranial Vault Remodeling
(Courtesy of Dr. Caitlin Hoffman)
“We are also using 3D imaging to define volumetrics based on the surgery that was performed and the suture that was fused,” explains Dr. Hoffman. “By looking at the rate of change in volumetrics, we can predict when an alteration in intraoperative decision-making is needed to either remove more bone or utilize additional bone removal strategies. 3D imaging also has a substantial advantage over CT – the only other tool that can currently provide this data – because we avoid exposing infants to ionizing radiation.”
A Training Model for Residents
Surgical procedures to correct craniosynostosis include cranial vault remodeling, fronto-orbital advancement (FOA), and endoscopic suturectomy – all of which require experience with complex anatomy and tools. However, neurosurgical residents rarely have exposure to these complicated procedures during their training. The craniofacial teams of Weill Cornell Medicine and Columbia therefore sought to establish a training experience that would better prepare residents, fellows, and junior attendings for performing these procedures and enhance their neurosurgical education and training.
To this end, they created a hands-on practical course in both open and endoscopic craniofacial approaches that utilizes novel 3D printed models fabricated from patient scans representing calvaria, soft tissues, and cranial contents. Over the past four years, this training method has evolved to incorporate the most innovative technical modalities, now with an international attendance to gain surgical skills through this approach. A comprehensive article describing the creation and application of the skull models in training courses was published in the December 2019 issue of the Journal of Neurosurgery: Pediatrics.
Is There a Role for Genetics?
Dr. Hoffman and her colleagues, in collaboration with the Greenblatt Laboratory and Ross Laboratory at the Weill Cornell Medicine Feil Family Brain and Mind Research Institute, have also begun to perform molecular analysis of actual bone, suture, and blood specimens to evaluate how this data may affect patient outcomes and help with discussions of parental expectations. “Dr. Matthew Greenblatt is investigating the potential cellular mechanisms that are responsible for these early fusions, and, in conjunction with Dr. Margaret Ross, we are looking into individual patients’ genomics and how these may interplay with these cellular mechanisms as well as a patient’s functional and morphologic outcomes. This would indicate which patients are better suited to an endoscopic approach versus an open approach and how that information relates to their ultimate outcomes,” notes Dr. Hoffman. “Our hope is that we learn how to be more predictive and more targeted in our therapies, thereby helping families to know what better to expect and achieve better outcomes in the long run.”
Identifying Disparities in Access to Craniofacial Surgery
In research published in the April 2021 issue of Neurosurgical Focus, Dr. Hoffman, Dr. Imahiyerobo, and their colleagues in the Departments of Neurosurgery and Plastic Surgery at Weill Cornell Medicine and Columbia, conducted a retrospective study to evaluate the impact of health disparities on access to treatment for children with craniosynostosis. The researchers reviewed the charts of children who underwent either open surgery or minimally invasive endoscope-assisted suturectomy at two tertiary care hospitals in New York City from January 1, 2014 to August 31, 2020. Of the 121 children identified; 62 had open surgeries and 59 underwent the endoscopic procedure.
Their findings showed health inequities among Black and Hispanic children who did not have insurance or had Medicaid status, as significantly more of these patients were treated in the open surgical group compared to the endoscopic group.
The authors note, “The results of our study demonstrate that Black and Hispanic patients presented later for initial consultation and therefore underwent surgical intervention at an older age.” Consequently, many of these patients were ineligible for endoscopic surgery and the clinical and psychosocial benefits it confers.
“It is important to make sure we are mitigating healthcare disparities,” says Dr. Hoffman. “We found a substantial difference for patients who were not referred early enough. We are working actively to mitigate these factors and be more attentive to healthcare access.”



