For Jacqueline Jossen, MD, treating celiac disease is both personal and professional. Dr. Jossen, a pediatric gastroenterologist and assistant professor of pediatrics at NewYork-Presbyterian/
Now, 10 years after her diagnosis, Dr. Jossen is one of two physicians leading the pediatric arm of Columbia’s Celiac Disease Center, the first program in New York City dedicated to the treatment of celiac disease. Celiac disease affects nearly 1 percent of people in the U.S., and treatment requires strict adherence to a gluten-free diet. “I always tell our trainees that if you’re treating a patient with celiac disease, you should try a strict gluten-free diet for a week and see what it’s like,” she says. “It’s really eye-opening.”

Dr. Jacqueline Jossen
Started in 2001 under the leadership of Peter Green, MD, the Phyllis and Ivan Seidenberg Professor of Medicine at Columbia, the Center offers a multidisciplinary and collaborative approach to managing the disease throughout the course of a patient’s life. “We facilitate the transition of these patients from pediatric into adult practice fairly seamlessly. Our dietitians are the same for both pediatric and adult. They are a really important conduit during that transitional period,” Dr. Jossen says. “We have world-renowned physicians and researchers so you know that when you come to the Celiac Disease Center, you’re going to be getting the care that’s the most up-to-date.”
Updates on the Diagnosis and Management of Celiac Disease
Traditional diagnosis of celiac disease in the United states includes serologic tests, specifically tissue transglutaminase immunoglobulin A (TTG IgA). If that test is positive, then patients undergo an endoscopy to take an intestinal biopsy to confirm the diagnosis. However, the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) has been using guidelines for diagnosis that forgo biopsy.
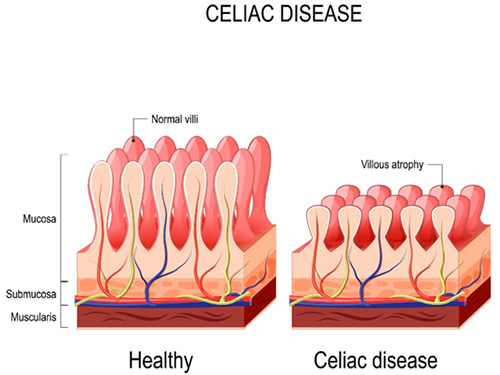
A comparison of a section of health small bowel compared to a section of small bowel showing villous atrophy caused by celiac disease.
“This is a very controversial and hot topic within pediatric gastroenterology,” Dr. Jossen says. “Essentially, if a patient walks into your office with certain lab parameters, you might be able to make a celiac diagnosis without biopsy based on these labs.”
Last year, Benjamin Lebwohl, MD, an adult gastroenterologist at NewYork-Presbyterian/

Dr. Benjamin Lebwohl
ESPGHAN recommends that if TTG IgA is over 10 times the normal limit for the lab, and you have a positive endomysial antibody (EMA) in a second blood sample, a biopsy is not needed to make a celiac diagnosis in children. The non-biopsy approach, which is based on prospective data in children, has been used in Europe since 2012. Dr. Jossen notes that there is fear within the pediatric community about use of these guidelines.
“Part of the fear is that these criteria will be applied incorrectly,” she says. “We don't want patients to be misdiagnosed, and we want to make sure they are able to establish care with a knowledgeable gastroenterologist and dietitian.”
Before the COVID-19 pandemic, the pediatric celiac community in the United States didn’t stand behind these guidelines. However, the pandemic changed patient care due to the temporary elimination of elective procedures. “We had no elective procedures and we were seeing patients who were coming in with very high TTG values and we were turning to them, and to ourselves, and saying ‘What are the chances that this patient doesn’t have celiac disease? Do we really need to wait several months to do an endoscopy? So, it was nice that we had these guidelines because we could use them and apply them in the telehealth setting,” Dr. Jossen says. “When elective endoscopy resumed, I think there was a greater willingness to accept these guidelines.”
Dr. Jossen notes that an important part of the guidelines is informed decision-making with the families. “A non-biopsy diagnosis requires that the family agrees with this approach,” she says. “I think that’s really important because they need to understand that if they want to go back for a biopsy later, that will involve a gluten challenge. Additionally, there’s a possibility that we will miss another disease by not doing the biopsy. All of these things are really important to talk to parents about before making this decision.”
Although she prefers diagnosing after doing an endoscopy, Dr. Jossen says she will diagnose a patient using that criteria after having the appropriate conversation with them.
Tackling Misinformation Regarding Celiac Disease and Gluten Sensitivity
The rise of popularity in the gluten-free diet has been drastic in the past decade. Drs. Jossen and Lebwohl recently coauthored an editorial in Digestive Diseases and Sciences aiming to educate other providers about non-celiac gluten sensitivity (NCGS). “It’s been popularized by the mass media and celebrities. And yet the research behind it is relatively sparse,” Dr. Jossen says.
In the article, Drs. Jossen and Lebwohl responded to a new study assessing NCGS highlighting claims about the gluten-free diet that are either unproved or have been refuted, including that “the diet is healthier, promotes weight loss, improves acne, alleviates gastrointestinal symptoms, or is effective as an adjunct treatment for autoimmune diseases.”
Dr. Jossen says that there are many people who place themselves on a self-prescribed gluten-free diet who may have something else that they haven’t been tested for that can be improved without the diet. “I think it’s really important to disseminate knowledge about what the actual science is here because there are so many patients coming in to providers’ offices saying ‘Oh I’m gluten sensitive.’ But what does that mean? That’s what we tried to address in the article,” she says.
Whereas those with celiac disease have been diagnosed using serologic and histologic biomarkers, NCGS is challenging to measure or confirm in clinical practice.
“The data suggest that the term NCGS used to describe the population with perceived gluten sensitivity in the absence of diagnosed celiac disease is a misrepresentation of the true nature of this syndrome. Rather, there is considerable heterogeneity in this population in terms of dietary triggers that should be accounted for when diagnosing and counseling patients,” the authors wrote.
Dr. Jossen notes that following a gluten-free diet comes with nutritional pitfalls. “The foods are not vitamin fortified like their gluten containing counterparts,” she says. “Following a patient [on this diet] is important, not sending them to live without any nutritional support.”
If there is suspected celiac disease, Dr. Jossen says its important that patients do not remove gluten from their diet. “All of our celiac disease testing 100 percent relies upon gluten being in the diet,” Dr. Jossen says. “So, if you suspect celiac disease in a patient, do not let them remove gluten from their diet. Get them to a gastroenterologist. It is always a challenge to sit with a patient and tell them about needing to reintroduce gluten for several weeks before I can make an accurate diagnosis. And that’s very challenging for a parent who feels like giving their child a slice of bread is essentially poisoning them.”
“If you suspect celiac disease in a patient, do not let them remove gluten from their diet. Get them to a gastroenterologist. It is always a challenge to sit with a patient and tell them about needing to reintroduce gluten for several weeks before I can make an accurate diagnosis. And that’s very challenging for a parent who feels like giving their child a slice of bread is essentially poisoning them.” — Dr. Jacqueline Jossen
Ongoing NewYork-Presbyterian Research in Celiac Disease
The Celiac Disease Center at Columbia University is currently conducting multiple trials for non-dietary therapies in celiac disease. In addition to clinical trials of these experimental treatments, the center is investigating parental and individual attitudes towards participation in celiac disease research. “[For pediatric patients], there is no treatment for celiac disease except a strict gluten-free diet,” Dr. Jossen says. “Clinical trials involving pediatric patients have to be specialized for those in that special population. These are patients who already have a treatment and whose parents may need to intentionally give their child gluten in order to forward research. Are they willing to do that? And if so, how far can we push it? We wanted to understand what parents would be willing to do and how they feel about their child participating in research.”
Columbia is also leading a study investigating pediatric provider attitudes toward a non-dietary therapy for Celiac disease. “Even within the medical community, many feel that it’s just a gluten-free diet,” Dr. Jossen says. “We know it’s so much more than that. This study is going to look at pediatric gastroenterologists and dietitians specifically to see how they feel about non-dietary therapy. Would they prescribe it? What will they consider to be important when making that decision?”
The team at Columbia is very focused on improving the quality of life in patients with celiac disease. In a research study looking at factors associated with maladaptive eating behaviors, social anxiety, and quickly of life in adults with celiac disease, Columbia investigators found that 39% of adults with celiac were afraid to kiss their partners for fear of contamination. Dr. Jossen says that they are in the process of conducting a follow-up study to evaluate this risk by measuring gluten in saliva following a kiss. “While the study will be conducted in adults, we are confident the results will also apply to our adolescent patients,” she says.



