Fetal surgery has earned its rightful place in the prenatal treatment of a number of congenital anomalies and continues to undergo rapid expansion, including for repair of myelomeningocele, the most severe form of spina bifida. The condition is associated with several complications, including early death, paralysis, and bowel and bladder dysfunction.
At NewYork-Presbyterian Morgan Stanley Children’s Hospital and Columbia, Neil A. Feldstein, MD, Director of Pediatric Neurological Surgery; Vincent P. Duron, MD, Co-Director of Fetal Therapy, Surgical Director of the Pediatric ICU, and Director of Minimally Invasive Surgery; Russell S. Miller, MD, Medical Director of the Center for Prenatal Pediatrics; and Lynn L. Simpson, MD, Chief, Division of Maternal Fetal Medicine, collaborate closely to optimize the fetal management of myelomeningocele.
In the Center for Prenatal Pediatrics at Columbia, neurological abnormalities are the second most common group of conditions seen after cardiovascular anomalies, and myelomeningocele is one of the most common birth defects seen by pediatric neurosurgeons. “Spina bifida develops early in fetal development during the third or fourth week,” notes Dr. Feldstein. “The vast majority of open neural tube defects occur in the lumbar and sacral region, and there is a huge disparity in outcomes for these children depending on the location of the defect. A few millimeters between the upper and lower lumbar spine can mean the difference in their ability to get in and out of a wheelchair, get up out of a chair, or walk up and down stairs. Because the lowest part of the spinal cord is frequently involved, nearly all of these children will have neurological and orthopedic issues, as well as bowel, bladder, and sexual dysfunction.”
The Role for Prenantal Intervention
Historically, spina bifida repair was performed in the first few days of an infant’s life. In 2011, the landmark trial, Management of Myelomeningocele Study (MOMS), showed that in utero fetal surgery dramatically improved the rates of hydrocephalus compared to surgery performed following birth. However, specialists in the field continued to grapple with high rates of maternal morbidity, including the increased risk of uterine rupture in subsequent pregnancies and maternal complications from a cesarean delivery.
“Prenatal intervention has been shown to significantly improve myelomeningocele outcomes by decreasing the need for cerebrospinal fluid shunting and improving motor function,” says Dr. Feldstein. “Our institution supported the findings of the Management of Myelomeningocele study, which showed that prenatal surgery significantly reduces the need to shunt fluid away from the brain. However, because open surgery is associated with risks to the fetus and mother, we wanted to explore other endoscopic surgical approaches.”
As the fetus grows, so does the neuro tube defect, making prenatal surgery more of a challenge the closer it’s performed to the birth. “Surgery performed after birth, however, is not particularly challenging because the visual field is exposed and you have access to operate from all directions,” explains Dr. Feldstein, who has taken care of hundreds of children with myelomeningoceles after birth. “About 80 to 90 percent of children with open neural tube defects born at term will develop hydrocephalus. And I can’t stress it enough, hydrocephalus is ultimately the undoing for so many of these children and adults. Once the hydrocephalus is present it becomes a lifelong concern managed by shunts to help drain the fluid. So, any intervention that can alleviate hydrocephalus will provide them with an incredible improvement in their quality of life.”
Dr. Duron concurs. ”The MOMS trial tested the hypothesis, ‘Is the prenatal repair advantageous when compared to the postnatal repair?’ The major finding from this trial, and the one that we emphasize to families, is the significant reduction in the need for a shunt following prenatal surgery. However, these positive fetal outcomes were counter-balanced by negative gestational and maternal outcomes. How do we weigh the maternal risks against the fetal benefits? Can we achieve safe maternal outcomes and fetal benefit at the same time? These questions were raised after MOMs and pushed the development of the fetoscopic minimally invasive technique.”
Fetoscopic Repair: Achieving Benefits for Both Mother and Baby
“We started by using the percutaneous approach but didn’t find it advantageous because there were still risks for maternal complication of premature rupture,” says Dr. Feldstein. “So we decided to pursue an alternative approach in which we deliver the uterus to perform the surgery fetoscopically. The fetoscopic approach is the best of both worlds. It minimizes the uterine opening and offers the most favorable benefit for the fetus.”
“The advantage of the externalization of the uterus is that sutures can be placed in a box configuration around where the ports are going to be placed,” says Dr. Duron. “This tacks up the membranes to the uterus to help prevent premature rupture. Another advantage of this approach is the possibility of vaginal delivery after fetoscopic repair.”
The fetoscopic surgery is typically performed between 19 and 26 weeks of gestation. Prior to the procedure, parents undergo extensive presurgical counseling, including meetings with the complete multidisciplinary team, so they are very well informed.
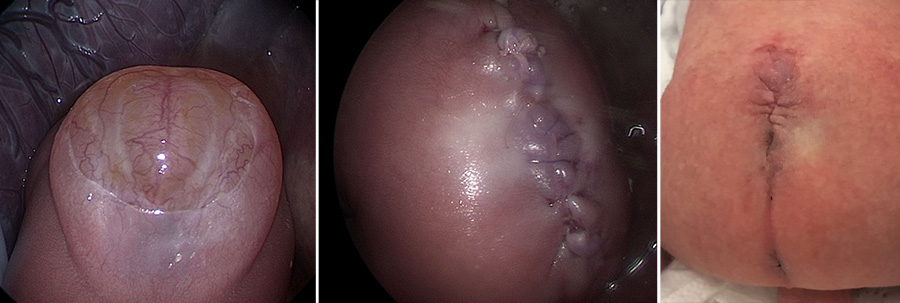
Fetal myelomeningocele defect, closure following fetoscopic procedure, and repair
“The uterus is externalized through an extended C-section type incision in the mother’s abdomen. The pediatric surgeon places multiple ports to visualize the infant and spinal cord defect,” explains Dr. Feldstein. “Dr. Duron and I do the repair and the team then puts the uterus back into the pelvis and the skin is closed.” The mother stays in the hospital for up to one week and returns for frequent follow-up visits to the Center for Prenatal Pediatrics during the remainder of her pregnancy. After the baby is born, the entire team follows the baby postpartum.
“As neurosurgeons, we need to recognize our capabilities and our limitations when we enter the OR,” notes Dr. Feldstein. “I am very comfortable with working through a ventricular scope, but this is very different from the instruments used in this type of surgery. I rely very heavily on my colleagues, especially Dr. Duron, who works with these instruments on a day-to-day basis. Whether it’s my hands or a colleague’s hands, we both have the same thought in mind on how to solve the problem. We all agree that when you recognize this is a group effort and each person’s specialty skills are brought to bear, the surgery proceeds beautifully. And that is what our team has experienced from the very beginning.”
According to Dr. Feldstein and Dr. Duron, the technically demanding procedure has a large learning curve, but the payoff is invaluable for babies and moms. “Before performing our first case, our team visited a very high volume center in Brazil, where we observed Dr. Denise Lapa perform a percutaneous fetoscopic procedure,” says Dr. Feldstein. “Dr. Lapa had spent years developing a way to repair spina bifida in the womb without making large incisions in the uterus or the abdomen in both animal models and clinical studies. She then came up to New York to help us with our first case, including providing hands-on training in our simulation lab.”
“We performed our first case on April 26, 2018, with a multidisciplinary team comprising maternal fetal medicine, pediatric surgery, pediatric neurosurgery, OB anesthesia, and our nursing team,” says Dr. Duron. “We work together, contributing each of our specific expertise to these procedures. From uterine access, to minimally invasive skills, to neuroanatomy and dissection, it really takes a team to be able to perform this procedure.”
Since then, the Columbia team has been performing fetoscopic surgery with great success, and they are now in a position to offer training in fetoscopic interventions.
“The reason this procedure can be performed here is because we have a comprehensive maternal fetal medicine program and clinicians very experienced with fetoscopy and taking care of complex prenatal patients,” says Dr. Duron. “It’s all about the infrastructure and having the experts in each field able to provide their skillset.”



