As a pediatric neurogastroenterologist, Julie Khlevner, MD, Director of the Pediatric Gastrointestinal Motility Center at NewYork-Presbyterian Morgan Stanley Children’s Hospital, provides highly specialized expertise for difficult-to-treat motility disorders in children. The emerging subspecialty recognizes the relevance of intestinal pathology and abnormal brain-gut interactions in neurogastroenterology and motility disorders. In a published review of the clinical implications of the brain-gut axis, Dr. Khlevner and her co-authors note that the relationship between the brain and the intestine begins during development and persists throughout life and, according to research studies, this is what links the emotional and cognitive centers of the brain with intestinal functions.
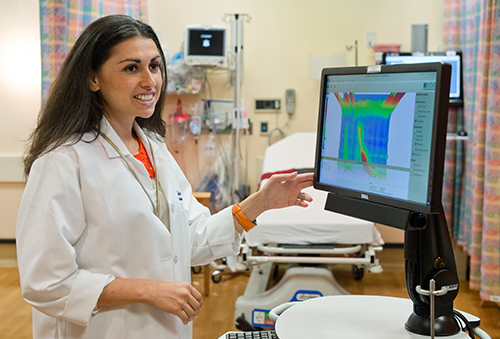
Dr. Julie Khlevner
The Pediatric Gastrointestinal Motility Center, established nearly a decade ago with Dr. Khlevner at the helm, provides a much-needed resource for infants, children, adolescents, and young adults whose motility conditions are often difficult to diagnose and challenging to treat.
“Motility disorders are non-discriminatory and can affect anyone regardless of age, ethnicity, or gender,” notes Dr. Khlevner. “Their etiology is multifactorial – whether genetic, idiopathic, or induced by surgery or other interventional procedures.”
In 2018, Dr. Khlevner was one of 35 leading experts invited to participate in a full day symposium on “Advances in Motility and in Neurogastroenterology – AIMING for the Future” held during the annual meeting of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. This symposium, which explored clinical paradigms in pediatric GI motility disorders, provided a foundation for advancing new scientific and therapeutic research strategies in the field.
Addressing Diagnostic Dilemmas
“Performing and interpreting motility evaluations in children present unique challenges that are further complicated by technical difficulties and patient cooperation,” notes Dr. Khlevner. “It's important to remember that pathophysiology of pediatric motility disorders can be very different than what's reported in adults. The lack of child-specific normative data can make analysis more difficult and care must be taken to avoid over-interpretation. For example, we often use Chicago classifications to diagnose esophageal motor disorders, but the normatives are based on adult data. Despite very few studies validating its use in children, we've applied these parameters to pediatrics.”
Functional gastrointestinal and motility disorders in children can range from relatively benign complaints, such as constipation, to more serious and rare conditions, such as Hirschsprung’s disease. Dr. Khlevner, in collaboration with multispecialty colleagues, provides comprehensive testing, consultation, and treatment with the goal of identifying the causes of a child’s symptoms and intervening to improve his or her quality of life.
“While upper gastrointestinal motility disorders are common in children, there's often a delay in diagnosing these conditions,” says Dr. Khlevner. “Children frequently present with nonspecific signs and symptoms that are often mistaken for gastroesophageal reflux. Many are prescribed acid-suppressant medications for a prolonged period of time before motility disorders are considered or undergo several invasive procedures that are non-revealing prior to considering an evaluation in a comprehensive motility program. A motility evaluation by an expert in the field plays an integral role in diagnosis when a workup is inconclusive and symptoms don't respond to conventional medical therapy. Motility disorders should always be considered in the differential diagnosis.”
Advances in technology to measure motor and sensory characteristics of the upper and lower GI tract have not only led to better understanding of the pathophysiology underlying neurogastrointestinal disorders occurring in childhood, they have also facilitated the development of less invasive diagnostic tests and more targeted treatment options. With resources that include the latest diagnostic and therapeutic tools, the Pediatric Gastrointestinal Motility Center is at the forefront of innovative evaluation and treatment.
Dr. Khlevner notes that esophageal manometry is a common procedure performed in pediatrics. “The advent of high-resolution manometry offers particular advantages for children because the study is easier to perform and provides unparalleled insight into esophageal physiology. With the addition of impedance to high-resolution esophageal manometry, the clinical significance of motor abnormalities can be assessed in the setting of effective or ineffective bowel clearance.”
The Motility Center also employs high-resolution 3D anorectal manometry, which is used to evaluate the voluntary and involuntary properties of the anorectum and to identify neuropathy in the setting of spinal pathology, as well as sitz marker studies to evaluate how quickly food is moving through the intestines.
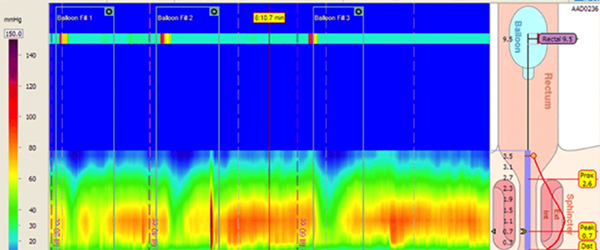
High-resolution 3D anorectal manometry in a 5-year-old boy with chronic refractory constipation. There is normal relaxation of the internal anal sphincter with each balloon inflation, ruling out Hirschsprung’s disease as a possible etiology for chronic constipation. (Courtesy of Dr. Julie Khlevner)
With the availability of evaluations by a neurogastroenterologist and the latest diagnostic tools in the field, the Motility Center attracts referrals from pediatricians and pediatric gastroenterologists from around the country.
Antroduodenal manometry is an advanced motility study that is less commonly performed but it has become important in the diagnosis of gastroparesis and pseudo-obstruction in children presenting with upper tract symptoms. Adds Dr. Khlevner, “As with esophageal manometry, high resolution manometry technology has also been applied. But more diagnostic tools that are validated in children are absolutely needed. Continued research of non-invasive diagnostic modalities may lead to less discomfort while maintaining a high degree of sensitivity and specificity for the diagnosis of these disorders.”
An Urgent Need for Child-Tested Treatments
“The pharmacotherapy currently available for pediatric motility disorders is very limited and new medications are certainly needed,” says Dr. Khlevner. “With limited treatment options approved for children, we often turn to off-label agents to help our pediatric patients.”
Current therapeutic procedures include Botox injections into gastrointestinal sphincters; biofeedback for the treatment of fecal incontinence; and specialized surgical procedures for motility disorders that are refractive to medical treatment.
“Importantly, our center participates in multicenter trials on novel pharmaceuticals not readily available elsewhere, which is particularly important for patients who have tried everything and nothing is effective.” — Dr. Julie Khlevner
“Hopefully, with the continued basic science advances in the function of the enteric nervous system, such as the identification of new receptors, new compounds will emerge and the treatment and prognosis of children with primary motility disorders will improve,” says Dr. Khlevner. “There are many promising treatments for children with motility and functional disorders in development, including regenerative medicine, optic genetics, and additional gut-selective medications.”
Setting Standards for Training in Pediatric Neurogastroenterology
As an emerging specialty, pediatric neurogastroenterology has been further strengthened with the development of guidelines for training in neurogastroenterology and motility disorders (NGM) under the auspices of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition and the American Neurogastroenterology and Motility Society.
In a collaborative effort with colleagues from 14 other centers, Dr. Khlevner led a joint task force of the two societies to identify the components of knowledge, skills, and management expected of NGM consultants and provide standards in training. The resulting document, published in the January 2021 issue of the Journal of Pediatric Gastroenterology and Nutrition was the first of its kind and has been endorsed by two major gastroenterology societies. The members of the task force anticipate that this document will serve as a resource to break existing barriers to pursuing a career in NGM and provide a framework towards uniform training expectations at three hierarchical tiers corresponding to EPA (entrustable professional activities) levels.
“The field of neurogastroenterology has received some much needed attention,” says Dr. Khlevner. “It is a vibrant and exciting specialty and the future is bright for children with these disorders.”



