Och Spine at NewYork-Presbyterian, led by Lawrence G. Lenke, MD, Chief of Spinal Deformity Surgery in the Department of Orthopedic Surgery at NewYork-Presbyterian/
In a recent study, Dr. Lenke and his colleagues at NewYork-Presbyterian/
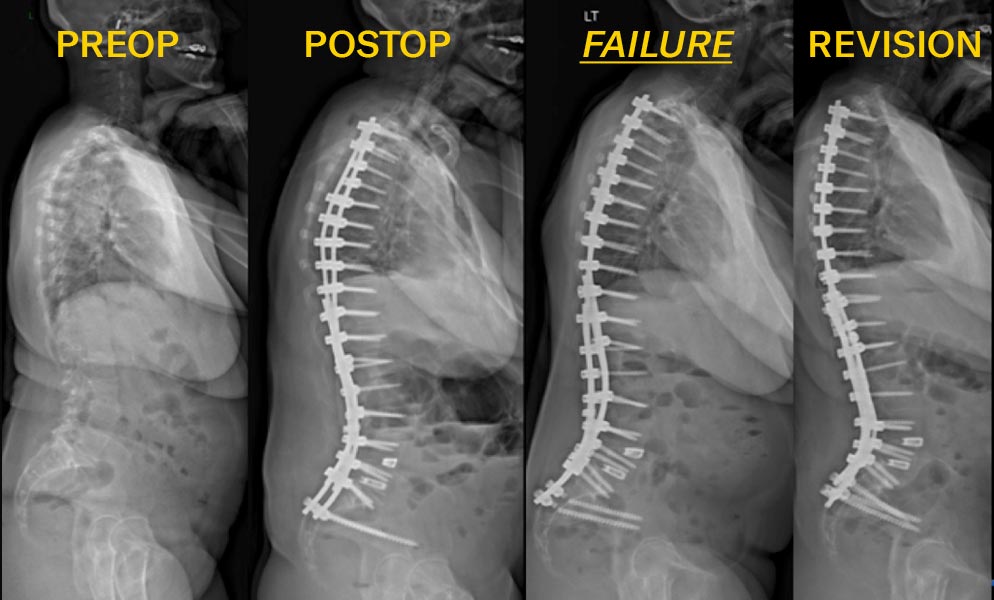
A 57-year-old female with adult idiopathic scoliosis who underwent posterior spinal instrumented fusion from T2 to Pelvis with interbody fusions at L4-5 and L5-S1. Postoperatively, she had pseudarthrosis with bilateral iliac screw fractures. Revision surgery included re-instrumentation from T11 to the pelvis with 4 pelvic fixation points, 5 rods spanning the lumbo-pelvis with accessory rods anchored distal to S1.
The researchers conducted a retrospective study of 253 adult patients 18 years of age or older who underwent spinal arthrodesis by five spine attending surgeons at Och Spine at NewYork-Presbyterian between 2015 and 2019. All patients had fusion of six or more operative levels with a combination of bone morphogenetic protein, local autograft, and allograft. Both primary and revision cases other than prior pelvic fixation were included with a minimum follow-up of two years.
The researchers’ definition of pelvic fixation failure was consistent with that used in prior literature – any revision to the pelvic screws within two years after the index surgery. Revision surgery might be necessitated by:
- Pseudarthrosis with or without broken rods across the lumbosacral junction
- Broken pelvic screws
- Loose pelvic screws
- Sacral or iliac fracture
- Rod displacement at the level of the pelvic screws
In their review, the research team accounted for the following operative and instrumentation factors, noting specific data for their cohort:
- Total instrumented levels – mean of 13.6
- Three column osteotomy – 15.8 percent
- Interbody fusion at L5–S1 – 74 percent
- Screw parameters: number of pelvic screws – mean of 2.3; all screws were close-headed / screw type – 70 percent had S2AI screws only; 15 percent had iliac screws only; 15 percent had both S2AI and iliac screws / length/diameter of pelvic screws – mean of 8.6/86.6 mm for left side and mean of 8.6/87.4 mm for right side / presence of dual-headed S1 screws – about 33 percent of the left side S1 screws and 45 percent of right side S1 screws were dual-headed
- Rod parameters: rod diameter – all rods were 6.0 mm in diameter / number of rods crossing the lumbopelvis – mean of 3.5; about 45 percent of patients had more than 3 rods crossing the lumbopelvis and 94 percent had more than 2 rods crossing the lumbopelvis / all rods were cobalt-chrome / presence of a kickstand rod – 17.8 percent / accessory rods – lowest instrumented vertebra (LIV) to S1 present in 41 percent of patients and LIV to S2/ilium present in 52.6 percent
Findings from the study, published in the October 14, 2022, issue of Journal of Neurosurgery Spine, demonstrated a pelvic fixation failure rate of 4.3 percent in the cohort of 253 patients at a mean of 515 ± 152 days after the index surgery – well below PFF rates reported in the literature. The following table presents the reasons identified by the Columbia faculty for patients requiring revision surgery for PFF.
| Reason for Revision | Number of Patients | Percent |
|---|---|---|
| Total | 11 | 4.3% |
| Reason for Revision | ||
| Broken rod across lumbosacral junction | 4 | 1.6% |
| Other pseudarthrosis across lumbosacral junction | 3 | 1.2% |
| Broken pelvic screw | 1 | 0.4% |
| Loose pelvic screw | 1 | 0.4% |
| Sacral or iliac fracture | 1 | 0.4% |
| Painful/prominent pelvic screw | 1 | 0.4% |
Our single-center study of 253 ASD patients demonstrated a two-year PFF rate of 4.3 percent at a mean of 515 ± 152 days after the index surgery. This PFF rate appears to be substantially lower than what has been reported in the literature.
— Study authors, JNS Spine
In their review, the Columbia team also discuss a number of studies in the literature that shed light on the issue of pelvic fixation failure, including potential risk factors such as large pelvic incidence, longer fusion constructs, revision surgery, and failure to optimize sagittal balance. They note, “After accounting for these risk factors as well as several additional radiographic and operative variables, the most influential protective factors were a higher number of rods across the lumbosacral junction and accessory rod LIV to S2 or ilium, which likely increase construct stiffness, and lower residual coronal malalignment.”