At the intersection of neurology, ophthalmology, and interventional neuroradiology, experts at NewYork-Presbyterian/Weill Cornell Medicine are making groundbreaking discoveries that illuminate the complexities of the brain-vision pathway and bring patients novel therapeutic approaches to improve vision and quality of life. Recently, Marc J. Dinkin, MD, Director of Neuro-Ophthalmology at NewYork-Presbyterian/Weill Cornell Medicine, and his colleagues conducted a meta-analysis of outcomes data for venous sinus stenting, one of several surgical treatments for idiopathic intracranial hypertension (IIH), a debilitating condition that can cause life-altering changes in vision. The findings confirm that venous sinus stenting is a viable treatment option for medically refractory IIH patients, especially when papilledema threatens their vision.

Dr. Marc Dinkin
“IIH is a rare condition characterized by an elevation of intracranial pressure caused by cerebral spinal fluid, and there is no tumor, bleed, meningitis or venous occlusion to otherwise explain the condition,” explains Dr. Dinkin. “Typically affecting women of child-bearing age who have an elevated body mass index, the symptoms of IIH include headache, transient loss of vision, double vision, and pulsatile tinnitus.”
To Dr. Dinkin, the most concerning symptom of IIH is papilledema, which can lead to secondary progressive optic atrophy, visual loss, and blindness. “Some studies show up to 25% of patients with IIH have permanent visual field defects, which can be life-altering and debilitating for these patients,” he says. “Because of this risk, we take IIH very seriously and do everything we can to mitigate progression of disease.”
Some studies show up to 25% of patients with IIH have permanent visual field defects, which can be life-altering and debilitating for these patients. Because of this risk, we take IIH very seriously and do everything we can to mitigate progression of disease.
— Dr. Marc Dinkin
Finding the optimal ways to treat IIH
For most patients, IIH can be effectively treated with a combination of pressure-lowing medicines, such as acetazolamide, and weight reduction. However, some patients do not respond to or cannot tolerate medical therapy.
“In patients with medically refractory IIH, we may consider a surgical option, especially if the patient has significant papilledema that is causing visual field loss and threatens to lead to a life-altering change in their vision,” says Dr. Dinkin. “Traditional surgical approaches to IIH include shunting (a ventriculoperitoneal shunt or a lumboperitoneal shunt), which serves as a conduit for cerebral spinal fluid away from the brain, and optic nerve sheath fenestration, in which the surgeon makes an incision in the dural covering around the optic nerve.”
While these surgical approaches can be effective, each has its own failure and complication rates. “Shunts can become occluded or infected, and they can sometimes drain too much fluid, leading to dangerously low intracranial pressure,” explains Dr. Dinkin. “Moreover, living with a shunt requires a major lifestyle change for patients because they can feel the tubing coursing under their skin.”
Although the underlying causes of IIH are not fully understood, in 2002 it was found that a vast majority patients with IIH have stenosis of the lateral venous sinuses. This discovery led to the exploration of venous sinus stenting in patients who have venous sinus stenosis on MRI or CT. The procedure involves the placement of a stent in one of the venous sinuses via a small incision in the groin area, thereby relieving the stenosis and the increased intracranial pressure to alleviate symptoms.
For nearly a decade, experts at NewYork-Presbyterian/Weill Cornell Medicine have been pioneers in developing, testing, and using venous sinus stenting to treat IIH. In 2016, Dr. Dinkin and Athos Patsalides, MD, conducted a one of the first prospective clinical trials demonstrating improvement of visual parameters following venous sinus stenting in medically-refractory or medially intolerant patients with IIH. The same year, a team of investigators including Dr. Dinkin, Dr. Patsalides, and Srikanth Boddu, MD, an endovascular surgical neuroradiologist at NewYork-Presbyterian/Weill Cornell Medicine, conducted a study that determined that venous sinus stenting can be an effective treatment for pulsatile tinnitus in patients with IIH. Subsequent studies showed significant improvement in intracranial pressure following the stenting procedure.
To increase knowledge among physicians about this promising treatment, the team recently conducted a meta-analysis to summarize the collective experience with venous sinus stenting for IIH that was published in the Journal of Neuro-Ophthalmology. “We hope these insights will help neuro-ophthalmologists, who are typically are on the frontlines taking care of IIH patients, consider this approach as a potential therapy for their patients.”
Results of the Meta-Analysis
The meta-analysis included 49 studies (45 retrospective and four prospective) and 18 case reports (with three or less patients), yielding a total of 1,626 patients. The investigators found that among the 250 patients in whom post-stent intracranial pressure was measured, the mean value of pressure was reduced from a mean of 33 cm H20 to 19.7 cm H2O. Additionally:
- Transient visual obscurations resolved in 79.6% of the 201 patients who complained of it
- Pulsatile tinnitus resolved in 84.7% of 515
- Diplopia resolved in 93% of 86 patients
- Nonspecific visual symptoms, such as blurry vision, improved in 76.2% of 537 patients
Headaches resolved in 36% and improved in 40.7% of 1,105 patients after stenting. Of 1,116 with papilledema, 40.8% showed resolution and 38.2% showed improvement. “When thinking about efficacy for IIH, the number one question is, what is the efficacy for papilledema, the main cause of vision loss in these patients?” says Dr. Dinkin. “This analysis showed that the vast majority of patients with papilledema had either resolution or improvement of their papilledema after stenting.”
When thinking about efficacy for IIH, the number one question is, what is the efficacy for papilledema, the main cause of vision loss in these patients? This analysis showed that the vast majority of patients with papilledema had either resolution or improvement of their papilledema after stenting.
— Dr. Marc Dinkin
“Another important test of efficacy is improvement of the visual field, which I believe is more important than resolution of other IIH symptoms such as headaches or pulsatile tinnitus because it demonstrates that the treatment is really working to prevent permanent visual loss,” continues Dr. Dinkin. “Of the 386 patients that had visual fields tested before and after stenting, 239 improved and only 17 worsened.”
The meta-analysis also explored complications associated with stenting, which included in-stent stenosis or thrombosis, subdural hematoma, intracerebral hematoma, cerebral edema, stent migration, and death. Additionally, 9% of patients experienced a recurrence of symptoms which required a follow-up surgical intervention.
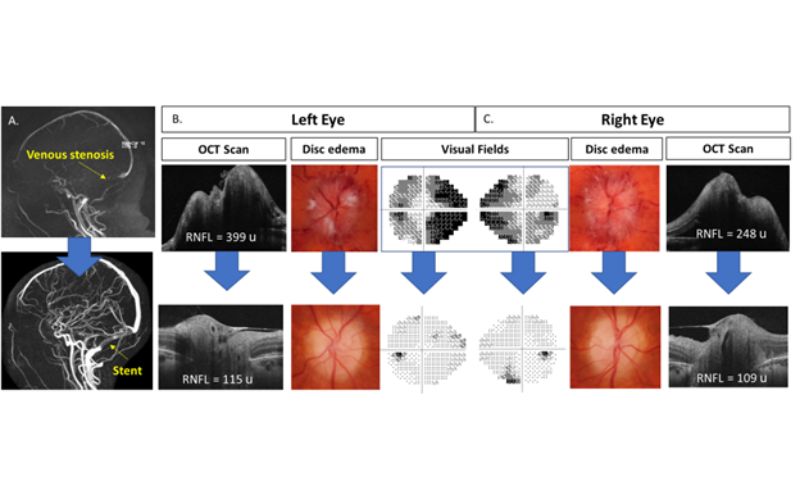
A woman in her 20s presented with severe headaches, episodes of missing vision when she stood up and whooshing sounds in her right ear. Neuro-ophthalmic examination revealed optic nerve swelling (papilledema) in both eyes. Formal visual field testing showed severe loss of peripheral vision in both eyes, while funduscopy demonstrated severe optic nerve swelling in both eyes. MR venogram revealed severe stenosis of the right transverse sinus. Lumbar puncture showed normal contents but opening pressure was very high at >55 cm of water. Due to ongoing severe visual field loss despite medical therapy with acetazolamide, a venous stent was placed in the narrowed venous sinus. (A.) Sagittal MRI showing the severe venous stenosis at presentation and the improvement in flow following placement of a venous stent. Improvement in optic disc edema, optic nerve thickness as determined by optical coherence tomography (OCT) and visual fields is seen in the left eye (B) and right eye (C). Headaches, episodes of vision loss, and whooshing all resolved.
“Some patients think that because venous sinus stenting is a neuro-interventional or radiological procedure and not a “surgery,” that it is not associated with potentially serious complications, but it can be,” says Dr. Dinkin. “For example, our analysis found a mortality rate of 0.036% related to the procedure itself. The rates of serious complications of stenting are quite similar to, if not slightly less than that of shunting, but they are not zero.”
The team concludes that venous sinus stenting is a viable and relatively safe option for medically refractory IIH, especially when papilledema threatens visual function. However, before stenting can be fully accepted as standard of care in the management of IIH, more research is needed.
“Many questions remain regarding about venous stenting for IIH, such as the true risk of complications and the risk and predictors of failure or recurrence,” says Dr. Dinkin. “These questions would be best answered by head-to-head prospective trials.”
Many questions remain regarding about venous stenting for IIH, such as the true risk of complications and the risk and predictors of failure or recurrence. These questions would be best answered by head-to-head prospective trials.
— Dr. Marc Dinkin
Multidisciplinary Collaboration for IIH
At NewYork-Presbyterian/Weill Cornell Medicine, Dr. Dinkin closely collaborates with a multidisciplinary team of specialists that includes Dr. Boddu, who applies the latest innovations in neuroimaging and stenting technology to improve outcomes in IIH patients, and Jeffrey Greenfield, MD, PhD, a pediatric neurosurgeon who is an expert in the management of CSF diversion procedures such as VP shunts.
“One novel imaging approach we are using to evaluate venous sinus stenosis is intravascular ultrasound (IVUS), a catheter-based technique that allows real-time, 360-degree visualization of the vessel and wall in three dimensions,” explains Dr. Dinkin. “The benefit of IVUS is that it offers a precise picture of the interior of the vein, so it improves diagnostic accuracy of the stenosis and helps us guide optimal stent placement.”
The team is also assessing novel stents that are specifically designed for venous sinus stenosis in the River clinical trial. “The majority of stents for venous sinus stenosis are off-label stents intended for the carotid artery, not for the vein,” explains Dr. Dinkin. “Weill Cornell Medicine is a major center for the River trial, a prospective, multicenter trial evaluating the safety and benefit of the novel River stent in patients with IIH. This stent is longer compared to other stents, to reduce the chance of requiring a second stent later. Additionally, It is more compliant than other stents, so it adapts better to the complex anatomy of the venous sinuses, and it has variable stiffness to adapt to the physiology of the stenosis of the venous sinuses.”
“At NewYork-Presbyterian, I feel really fortunate to work with talented fellow neuro-ophthalmologists like Cristiano Oliveira, MD, and John Paddock, MD, and highly trained neurosurgeons, like Dr. Boddu and Dr. Jeffrey Greenfield, who are careful and technically successful practitioners and make themselves an integral part of the care team for our IIH patients,” says Dr. Dinkin. “We are now planning a prospective trial of shunting versus stenting in patients with IIH. We all have the same goal, which is to prevent vision loss and improve the lives of our patients.”