In patients with refractory ulcerative colitis, and a subset of patients with Crohn’s disease, the gold standard surgical treatment is a restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA), commonly referred to as a J-pouch. According to David Schwartzberg, MD, FACS, FASCRS, a colorectal surgeon who specializes in J-pouch & redo J-pouch surgery at NewYork-Presbyterian/Columbia, most patients who undergo this procedure do extremely well. However, there is also a subset of patients who, unfortunately, do not. “These patients have symptoms of pouch failure, and that area is obscure not only for patients but healthcare providers as well,” he says. “It’s very frustrating for the patient when they are not living the life they expected after J-pouch surgery, meaning their pouch is not functioning as they were told it would, or they still require medical and surgical interventions to treat their symptoms, but the way I approach these patients is, ‘what is the underlying problem that is causing these symptoms, and how can I fix it?’”
Dr. Schwartzberg is dedicated to understanding pouch function and chronic pouch conditions so that he can find the best ways to treat each individual patient’s unique needs. “For a long time, any issues in a patient with a J-pouch were considered to either be pouchitis or pouch failure,” he says. “The thinking has been that if you’re having pain, or you have chronic pouchitis, then you must have Crohn’s disease. And, since no one ever disproves that assumption, the patients get told there are two options – either we give you a biologic medication, which is one of the things that the patient thought they were not going to have to take anymore, or they need a pouch removal because the feeling is that someone with Crohn’s disease can’t have a pelvic pouch. We need to look at the symptoms they are experiencing and take time to figure out what is causing them. What’s causing abdominal pain, chronic pouchitis, the inability to eat, the pelvic pain, what’s causing fevers or obstructive defecation, and more. It is only then that we can hopefully correct the underlying problem.”
Identifying the alternative causes of chronic pouch conditions
While pouchitis and pouch failure can occur in patients with a J-pouch, many times there are underlying causes of these conditions that can be treated if they are recognized. “It’s kind of this big mystery where, if you’re able to really understand the pouch and how the pouch is created, the pitfalls and possible complications of pelvic pouches, then you may start to be able to figure out what’s wrong with the pouch, or if it’s something other than the pouch that is causing these symptoms,” Dr. Schwartzberg says.
Some J-pouch patients experience chronic abdominal pain, inability to eat, and intestinal obstructive symptoms. For years, patients with these symptoms were labeled as having “pouch failure” and abdominal causes of their symptoms were ignored as diagnostic and treatment efforts are focused specifically on the pelvic pouch. However, Dr. Schwartzberg asserts that patients with J-pouches must be considered for abdominal pathology as well. Potential abdominal causes of these symptoms include afferent loop syndrome, anastomotic stricture at the ileostomy closure site, a non-functional side-to-side stapled ileostomy closure site, chronic adhesive bowel obstruction, and intestinal fistulae from post-operative abdominal complications.
At the 2023 Advances in IBD Conference, Dr. Schwartzberg presented an abstract that shared a retrospective review of patients that were labeled as pouch failure who underwent medical and endoscopic therapy for symptom control after being referred to NewYork-Presbyterian/Columbia. All the patients had bowel urgency, multiple bowel movements (9-30/day), abdominal pain, oral food intolerance, and weight loss. These patients, who all had previously underwent multiple endoscopic procedures and treatment with biologic medications, had strictures and angulation in the small intestine (proximal to the pouch) found on pouchoscopy.
These patients ultimately required surgery and the findings were consistent with abdominal causes of their symptoms, not the pouch. Findings during surgery included a small bowel fistula with stricture and obstruction, a non-functional side-to-side stapled anastomoses with near-complete luminal obliteration and a fistula from a leak from the previous ileostomy site to the pouch-inlet.
All patients underwent a diverting stoma with bowel resection(s), and one patient had a pouch-inlet strictureplasty. Postoperatively, all patients had resolution of their abdominal pain and obstructive symptoms.
“This small retrospective review showed that we need to be thinking about abdominal issues and not jump directly to labeling everything as pouch failure,” says Dr. Schwartzberg. “These patients had abdominal issues, such as a stricture or scar tissue causing a chronic obstruction, but, because these patients have a pelvic pouch, it’s immediately labeled as a pouch issue and basically all efforts are forgone to identify anything other than a pouch problem.”
Educating providers about alternative causes for pouch issues
Dr. Schwartzberg is passionate about educating gastroenterologists and colorectal surgeons about other potential causes for pouch issues. He is a coauthor of a new quarterly column – The Pouch Corner – within the Inflammatory Bowel Diseases journal that explores pouch issues in depth, providing both medical and surgical perspectives, which is critically important.
“I think there are two important things, one is to be humble and take the time to really listen to the patient, and the other is to always be in a multidisciplinary setting because it’s important to see these patients and discuss them with their gastroenterologist, radiologist, nutritionist, and stoma nurses,” says Dr. Schwartzberg. “A lot of these issues are not easy to diagnose as a lot of these symptoms overlap with other symptoms. If someone is having symptoms that are consistent with pouch failure…we start from scratch. We examine previous pathology specimens, operative reports, postoperative courses and, most importantly, listen to the patient to understand the timing of symptoms. Patients who have years of normal pouch function, and then develop symptoms, may in fact have Crohn’s of the pouch, and medical therapy might be the appropriate treatment. However, patients who developed symptoms within a year or two after pouch surgery often have a mechanical/structural complication that can be corrected with surgery, a redo pouch.”
Complex cases require specialized care
Dr. Schwartzberg urges that these complex patients either seek care at an institution with a specialized IBD program and encourages providers to refer these cases to places like NewYork-Presbyterian/Columbia. “We are really one of the few places that can offer corrective surgery for J-pouch patients, more commonly referred to as a ‘redo pouch,’ but this is a little misleading as redoing the pouch might not involve removing the prior pouch, but simply fixing it,” says Dr. Schwartzberg. “That is important as many patients want to avoid losing intestine.”
Dr. Schwartzberg further asserts, “Patients with signs of pouch failure are often recommended to go back to a permanent ileostomy, which is an option if they want it. However, if the patient wants to avoid an ileostomy, they deserve an evaluation and assessment to see if a redo pouch is possible before simply moving forward with a pouch excision.”

Intraoperative photo of a redo J pouch for retained rectum. The pouch was salvaged and the proctectomy was completed.
The reason for the need for experienced, multidisciplinary care is because of the complicated and confusing ways these complications can present. “For instance, some people have a leak at the tip of J-pouch, which creates a very insidious infection,” he says. “It’s very hard to identify but once you do, it can be fixed without a fill pouch mobilization, and this may not even require a temporary ileostomy. The same thing goes for afferent limb syndrome, when the bowel gets stuck behind the pouch and causes obstructions. I have been able to fix these laparoscopically as well, which really minimizes postoperative pain.”
Another example of a complex pouch condition is pouch-twist. “The pouch is twisted 180 or 360 degrees and connected to the anal canal and patients have chronic bowel obstruction symptoms,” Dr. Schwartzberg says. “In this scenario, you must completely mobilize the pouch, disconnect the pouch from the anal canal, untwist it and reconnect it in the proper orientation. In other cases, when there has been a leak at the connection from the pouch to the anal canal, it can cause such a severe infection that the pouch ultimately must be excised, but we can make a make a new one and reconnect it to the anal canal. Thus, avoiding a permanent stoma for the patient.”
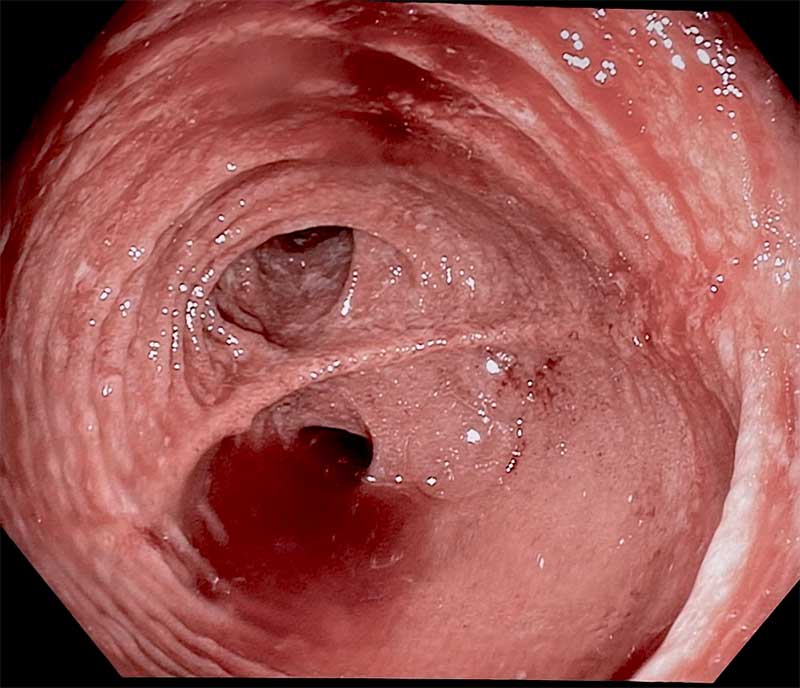
With the patient in lithotomy position, there is evidence of a pouch twist.
In other instances, pouch complications may be able to be treated endoscopically. At NewYork-Presbyterian, Bo Shen, MD, Director of the IBD Center at NewYork-Presbyterian/Columbia, has built an interventional IBD program that offers a middle option for patients between medical and surgical therapy. “Being taught by Dr. Shen personally, he and I have had success endoscopically fixing structural pouch issues in attempts to save the patient from having a very major surgery – a redo pouch,” says Dr. Schwartzberg. “We always attempt an endoscopic minimally invasive approach first.”
NewYork-Presbyterian/Columbia is a destination for the treatment of pouch complications. “Patients fly in from all over the world to see if they can avoid a permanent ileostomy or avoid surgery in general,” he says. “Our gastroenterologists and colorectal surgeons can offer advanced approaches that help them get their life back. So, if a physician is scratching their head and can’t figure out why a patient with a J-pouch isn’t doing as well as they should be, we would love to aid in the workup and to give additional options to those patients.”




