The field of bariatric metabolic surgery continues to evolve as new procedures emerge demonstrating improved benefits and reduced risks. Columbia and Weill Cornell gastroenterologists and GI surgeons are at the forefront of pioneering weight loss techniques and continue to refine minimally invasive approaches to advance the field.
Sleeve Gastrectomy versus Roux-en-Y
Metabolic problems associated with obesity have been a primary focus of bariatric surgeons for years and, in the last decade, the understanding of how surgical interventions can favorably alter metabolism has increased. In general, weight loss surgery can achieve diabetes remission, but the Roux-en-Y gastric bypass and duodenal switch have been shown to be the most effective procedures for diabetes control.
Columbia GI surgeons collaborate with endocrinologists on clinical initiatives, as well as studies seeking to improve outcomes of patients challenged by obesity. They were among the first to characterize the role of hormonal changes from the gut, especially the PYY effect, and they continue to actively study the duration of these effects and other outcome-related factors.
They have demonstrated in research studies that the anti-diabetes effect of certain bariatric procedures – particularly gastric bypass surgery – results from mechanisms that go beyond weight loss, supporting the use of this approach for treating type 2 diabetes.
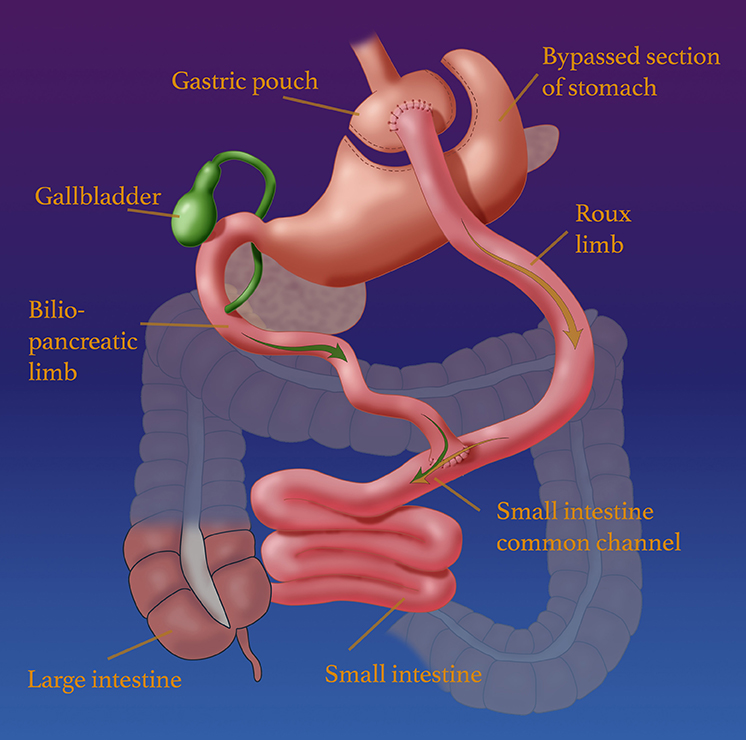
Medical illustration of Roux-en-Y gastric bypass
In a study published in the February 2019 issue of Science Reports, they compared sleeve gastrectomy, which is growing in favor today, with Roux-en-Y gastric bypass. According to the researchers, some randomized trials have shown lower weight loss and HbA1c improvement with sleeve gastrectomy compared with gastric bypass. Their study objective was to compare changes in beta-cell function following both procedures in patients who are obese and have type 2 diabetes with similar weight loss.
Patients undergoing sleeve gastrectomy were studied with an intravenous glucose tolerance test before surgery and at 5 to 12 percent weight loss post-surgery. They concluded that both sleeve gastrectomy and gastric bypass improve beta-cell function in the short term in obese patients with type 2 diabetes when assessed using an IV glucose challenge. However, further studies are needed to determine if longer-term clinical outcomes tend to be better after gastric bypass due to greater weight loss and/or other factors that differ between the procedures as a consequence of the different anatomical alterations.
In a study published in the July 20, 2020 issue of PLOS ONE, the Columbia research team investigated the differences in the effect of sleeve gastrectomy and Roux-en-Y gastric bypass on gastrointestinal hormones that regulate energy homeostasis. Their focus was on the roles of PYY, glucagon-like peptide-1 (GLP-1), and ghrelin for regulating glucose homeostasis and energy balance. By prospectively quantifying blood levels of gut hormones of energy and glucose homeostasis at one-year follow-up, they demonstrated significant changes after bariatric surgery in levels of the gut hormones that regulate glucose and energy homeostasis. Increases in postprandial PYY and GLP-1 levels in the blood were observed primarily after the Roux-en-Y procedure and transiently after sleeve gastrectomy.
The researchers concluded that differences in gastrointestinal hormones of energy homeostasis and changes in sweet cravings are possible mechanisms for greater weight loss and may mediate weight-independent improvement in insulin resistance after Roux-en-Y gastric bypass.
Five-Year Outcomes of Endoscopic Sleeve Gastroplasty
Weill Cornell gastroenterologists have conducted a prospective cohort study of 216 patients who underwent ESG from August 2013 to August 2019 to assess the long-term safety and efficacy of endoscopic sleeve gastroplasty (ESG) for the treatment of obesity. All procedures were performed by the same therapeutic endoscopist.
Patients with a body mass index of >30 kg/m2 or >27 kg/m2 with comorbidities were included in the study. At five years, the mean total body weight loss (TBWL) was 15.9 percent; 90 percent of patients maintained 5 percent TBWL, and 61 percent of patients maintained 10 percent TBWL.
While endoscopic therapies for weight management with ESG has been growing in popularity, its long-term outcomes had not been previously studied. The results of the Weill Cornell study suggest that endoscopic sleeve gastroplasty is a safe and reliable treatment option for obesity with durable long-term results.
Addressing GERD After Bariatric Surgery and as a Symptom of Obesity
Sleeve gastrectomy is the most common bariatric operation in the United States, but it is associated with increases in the incidence of gastroesophageal reflux disease (GERD).
A Role for Robotic-Assisted Surgery
Faculty in Weill Cornell’s tertiary-care bariatric center have used robotic-assisted management of intractable GERD after sleeve gastrectomy, describing their experience in the June 22, 2020 online issue of Surgical Endoscopy.
Calling on their prospectively maintained database, the researchers conducted a systematic review of consecutive patients undergoing robotic-assisted magnetic sphincter augmentation placement after sleeve gastrectomy (MSA-S group) or conversion to Roux-en-Y gastric bypass (RYGB group) for GERD from 2015 to 2019. These were compared to a consecutive group of patients undergoing robotic-assisted magnetic sphincter augmentation placement (MSA group) for GERD without a history of bariatric surgery from 2016 to 2019. The primary outcome was perioperative morbidity. Secondary outcomes were operative time, 90-day re-intervention rate, length of stay, symptom resolution, and weight change.
Of the 51 patients included in this study – 18 patients in the MSA group, 13 patients in the MSA-S group, and 20 patients in the RYGB group – BMI was significantly higher in patients undergoing RYGB compared to MSA or MSA-S. There were significant differences in operative time between the MSA and RYGB groups and the MSA-S and RYGB groups, but not between the MSA groups, nor was there a significant difference in intraoperative and postoperative morbidity. Furthermore, there was no difference on PPI discontinuation among groups, with more than 80 percent success rate in all.
The authors conclude that the use of the robotic platform in the different approaches available for treatment of GERD after sleeve gastrectomy appears to be a feasible option with low morbidity and high success rate, with further data needed to support their findings.
Endoscopic Sleeve Gastroplasty and Transoral Incisionless Fundoplication in One Session
Weill Cornell gastroenterologists have also evaluated the potential of performing endoscopic sleeve gastroplasty (ESG) and transoral incisionless fundoplication (TIF) in the same session as a possible solution to this common problem.
Their first case using this approach was a 63-year-old woman with class II obesity who was unable to lose significant weight with intensive lifestyle changes. She was on double-dose PPI for her reflux symptoms but did not experience sufficient relief. The GI surgeons performed TIF first, followed by ESG resulting in a tubular configuration of the stomach with a markedly reduced gastric body volume.
The total procedure time was 67 minutes: 24 minutes for TIF; 44 minutes for ESG. The patient was discharged home after endoscopy without any adverse events. She was maintained on a full liquid diet for the first three weeks. At the two-month follow-up, the patient reported a 43-lb weight loss (18 percent total weight loss) and two inches off of her waistline, with no reflux symptoms on a daily PPI.
Weill Cornell faculty note that endoscopic therapies have emerged to serve an unmet need in obesity and GERD therapy and are safe and effective when used with dietary and lifestyle changes. They emphasize the importance of appropriately selecting patients for these procedures with a multidisciplinary team. This was the first time same-session ESG and TIF has been reported. The procedure, which can be viewed on video in the July 9, 2020 issue of VideoGIE, demonstrates its safety and viability as a tailored approach in the treatment of obesity and GERD that occur concurrently.
On the Horizon
Columbia researchers are currently developing an endoscopic approach in animal studies and have designed a device aimed to mimic a gastric bypass completely endoscopically that is reversible and diverts the food from the esophagus straight to the intestine, bypassing the stomach and the duodenum. In their early trials in animals, it has shown to be very effective. They are now building prototype devices and expect to plan a human trial in the next year or so. Their goal is to develop endoscopic therapies that are as effective and yet safer and more easily reversible than surgery.



