Among the most challenging questions that David I. Kutler, MD, Director of the Division of Head and Neck Surgery in the Department of Otolaryngology at NewYork-Presbyterian/

Dr. David Kutler
“To be quite honest,” says Dr. Kutler, “there currently are no conclusive answers. In some patients, the lesion will remain pre-cancerous and other times the dysplasia progresses to cancer. We have no way to determine if someone is going to progress to cancer.”
This untenable clinical circumstance became the impetus for research by Dr. Kutler and his colleagues at Weill Cornell Medicine to uncover the genetic underpinnings that might shed light on these oral, potentially malignant, disorders. Their focus was on uncovering genetic changes that could cause atypical cells to transition to squamous cell carcinoma – a diagnosis with a five-year survival rate that has remained essentially unchanged for several decades despite advances in treatment.
“Currently, physical examination is the only tool we have for following these oral pre-cancerous lesions,” explains Dr. Kutler. So, Dr. Kutler and his team “initiated this study to determine if, by using RNA-seq technology, we could identify genetic changes occurring within the dysplasia that could definitively predict cancer transformation.”
Supported by an R01 grant in the laboratory of Lorraine J. Gudas, PhD, Chairman and Revlon Pharmaceutical Professor of Pharmacology and Toxicology at Cornell University, the researchers performed global transcriptomic analysis of tongue lesion samples from 20 patients treated at NewYork-Presbyterian/Weill Cornell Medicine. Nine patients had an oral potentially malignant disorder (OPMD) and 11 patients had squamous cell carcinoma (SCC).
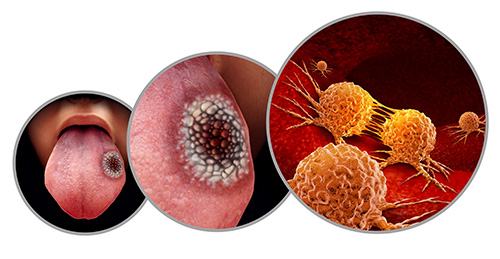
3D illustration of of squamous cell carcinoma
“We know that the histopathological characteristics of OPMD do not always accurately predict the clinical outcomes of these lesions,” says Dr. Kutler. “The goal of our research was to develop a signature gene set in which transcript level changes in an individual patient with these disorders could be used to predict the risk of developing squamous cell carcinoma. While many studies have looked at several different sites within the head and neck region, our study focused specifically on oral cavity dysplasia. What also distinguishes our study from others is that we analyzed both margin samples paired with the cancerous or pre-cancerous tissue from the same patient. This enabled us to compare the differences between the margin, which is normal, with the corresponding cancerous or precancerous lesion within the same patient.”
The results from this comparison provide novel molecular markers that may predict the risk of oral potentially malignant disorders becoming oral squamous cell carcinomas (OSCCs) and have the potential to improve early diagnosis and treatment decisions for OSCCs.
— Study authors, Discover Oncology
For this study, all lesions underwent a histopathologic examination followed by total RNA preparation and RNA-seq carried out in the Genomics Resources Core Facility at Weill Cornell Medicine. The findings, which were published in the February 23, 2023, issue of Discover Oncology, showed that:
- Transcripts altered in pathways in human tongue lesions at different stages are associated with pathological stages of the tongue lesions
- Gene expression profiles of human tongue lesions at different pathological stages indicate transcripts involved in human oral SCC progression
- Compared to margin tissue, SCCs showed more transcript changes than OPMDs
- The number of changed transcripts resembling human oral SCC molecular features in the OPMD samples is lower than that in the SCC samples indicating, as expected, that OPMDs display early pathological changes that may lead to SCC development
- Changes in gene expression profiles in individual patients categorized OPMD and SCC lesions into distinct subclasses similar to those seen in human head and neck SCC
- Both OPMDs and SCCs showed altered signaling pathways related to cell migration, basement membrane disruption, and metastasis
Dr. Kutler and his colleagues surmise that the subclasses of OPMDs – mesenchymal, basal, classical, and atypical – have the potential to be used to stratify patient prognoses and therapeutic options for tongue OPMDs. “We have identified a gene set whose transcript changes have the power to classify OPMDs and SCCs and developed a Firth logistic regression model using the changes in these transcripts relative to paired normal tissue to validate pathological diagnosis and potentially predict the likelihood of an OPMD developing into SCC,” the study’s authors conclude.
“While it is too early to apply the study’s findings to clinical practice and larger studies are needed, the implications for patient care are important,” says Dr. Kutler. “By characterizing the genes that are altered, we will be able to determine whether the lesion is going to progress to cancer, how aggressive the cancer is, and whether surgery, radiation, and/or chemotherapy are indicated. Essentially, we are looking for markers that will allow us to personalize the specific tumor so that we can personalize the treatment.”




