Download the Full Report View the E-booklet
Read more about our top research and key innovations from 2025:
Proven Treatments Remain Underused In Schizophrenia Care
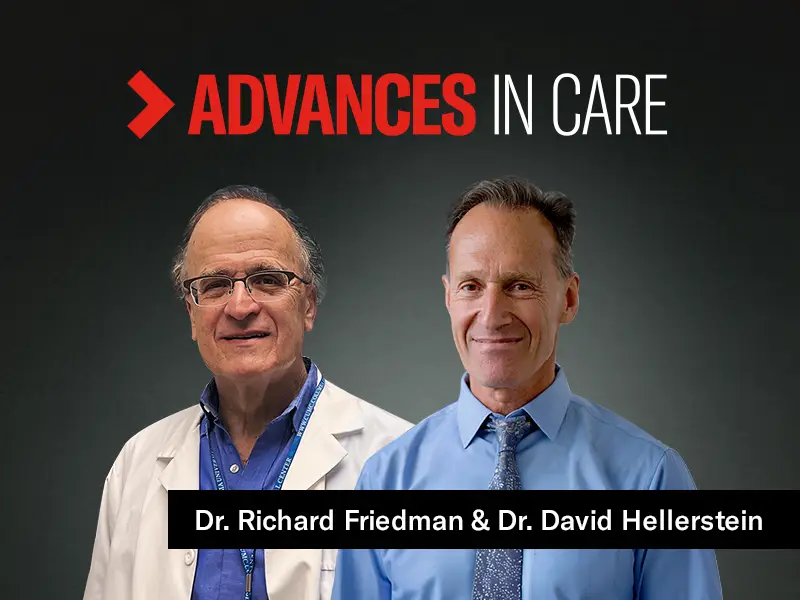
New Anxiety Treatment Pathway Could Eliminate Cognitive Side Effects
Addressing Concurrent ADHD In Alcohol Use Disorder
Endocannabinoids Reduce Opioid Reward Without Affecting Pain Relief
AI Model May Help Predict Onset Of Schizophrenia After Early Psychosis
Addictive Screen Use Linked To Suicidal Behavior In Adolescents
Exploring Psychedelics As The Next Wave Of Psychiatric Innovation