Epileptic activity during and between seizures in young patients may disrupt the development of neural networks beyond that expected from the underlying cause of the epileptic activity. Pediatric epilepsy can cause encephalopathy — manifesting as cognitive and behavioral impairments — and may disrupt normal brain development. Understanding and controlling pediatric seizures effectively and as early as possible is imperative to minimize their adverse effects on the developing brain, concluded NewYork-Presbyterian/Columbia pediatric epileptologists and neurologists in a recent review in the January 2024 issue of Pediatric Neurology.
"When managing epilepsy in children, the goal isn't just to address the seizures. It's about optimizing neurodevelopmental outcomes," asserts Columbia pediatric epileptologist Tristan Sands, MD, PhD, a pediatric epileptologist at NewYork-Presbyterian/Columbia and a lead author on the paper. "While we address quality of life for all patients with epilepsy, a really prominent aspect of children's care has to do with their brain development."
In the review, Dr. Sands and his co-author Jennifer Gelinas, MD, PhD, a pediatric neurologist at NewYork-Presbyterian/Columbia, address:
- Challenges in distinguishing epileptic encephalopathy (EE) from developmental encephalopathy
- Experimental evidence regarding mechanisms for EE development
- The differentiation between symptoms of EE and side effects of antiseizure medications
- The role of genetic testing in the clinical management of unexplained epilepsy
- Opportunities to modify epileptic activity to improve cognitive and behavioral outcomes
When managing epilepsy in children, the goal isn't just to address the seizures. It's about optimizing neurodevelopmental outcomes.
— Dr. Tristan Sands
Epilepsy and Encephalopathy
When epilepsy is accompanied by encephalopathy, it can be difficult to know whether the epilepsy is driving the encephalopathy, whether an underlying cause is responsible for both the epilepsy and the encephalopathy, or if both situations are present.
Examples of conditions in which epileptic activity can affect developmental outcomes in children include West syndrome, Dravet syndrome, Rasmussen encephalitis, and developmental and EE with spike-wave activation in sleep. Effectively treating epileptic activity during and between seizures may not only ameliorate symptoms but have a disease-modifying benefit that improves the developmental trajectory.
Mechanisms Behind Epileptic Encephalopathy
Preclinical models are helping researchers understand the roots of EE. Some studies have demonstrated that severe seizure activity in rodents results in persistent alterations and neural firing within regions of the brain associated with memory, as well as in neocortical regions. Early seizures in rodents can cause long-term abnormalities in social behavior and a tendency toward anxiety. Laboratory studies suggest that seizure activity in the developing brain can chronically shape the function of neural networks.
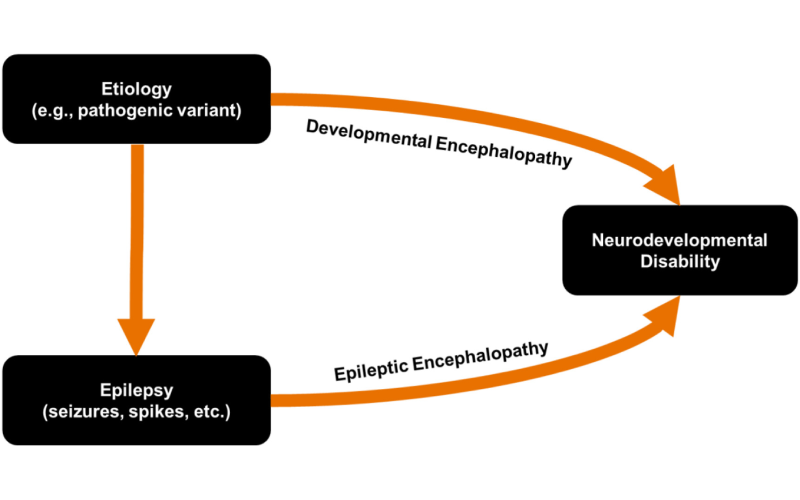
Diagram showing conceptual framework for the relationships between epilepsy and encephalopathy. (Image from Pediatric Neurology)
Epileptic activity involves coordinated neural firing that leads to pathologic high-frequency oscillations, which have been linked with memory and learning processes. Alterations in this frequency band during critical periods of brain development may impair the machinery required to promote intact cognitive functioning. In addition, preclinical data support the concept that seizures can lead to neuronal injury in the immature brain.
In a perfect world, antiseizure medications would exert their effects only when neurons are doing what we don't want them to do. But the truth is that they have effects that can contribute to behavioral dysregulation.
— Dr. Tristan Sands
Symptom Management vs Medication Side Effects
The side effects of antiseizure medications, which are typically used in combination for patients with refractory epilepsy, may further complicate clinical management. "In a perfect world, antiseizure medications would exert their effects only when neurons are doing what we don't want them to do. But the truth is that they have effects that can contribute to behavioral dysregulation and slow processing speed," explains Dr. Sands. "Many drugs dampen excitation in the brain and can make children sort of sedated. With difficult-to-control seizures, where we often combine multiple medications, we can really start to run into issues for children."
Observing the outcomes of children who have had surgery for refractory epilepsy can help tease out these effects. Removing a dysfunctional part of the brain has been shown to improve overall brain function, including cognitive function. The sooner a child with refractory epilepsy undergoes surgery, the better the outcomes. "For many of these patients, we are able to reduce the number or doses of medications or even enable them to stop taking medication altogether," says Dr. Sands. "The surgery itself can help children improve developmentally. But some of this improvement is related to being able to reduce their medications or eliminate them completely."
Achieving the right balance of medications and their doses is not an exact science. "The selection of medications, how to combine them, and knowing when to do surgery is all part of the art of epilepsy medicine," Dr. Sands adds.
The Value of Genetic Testing
Many of the causes of epilepsy have their roots in genetics. There are hundreds of genes that might play a role, and when they change, they can cause major issues for neurodevelopmental and motor development. In Dr. Sands' laboratory, he and his team are studying ways to target genetic changes that may trigger epileptic seizures. Their goal is to treat the underlying cause of the disease, rather than just managing symptoms. Even though this type of targeted therapy is not yet available for most genetic epilepsy, identifying the underlying genetic cause of epilepsy still leads directly to changes in clinical management in many cases, as demonstrated by Dr. Sands and colleagues in Epilepsia in 2023. The National Society of Genetic Counselors has recommended genetic testing for all patients with unexplained epilepsy to inform clinical management.
In 2016, he and his colleagues published a seminal paper in the journal Epilepsia regarding the treatment of self-limited neonatal epilepsy (SeLNE), a rare autosomal-dominant condition that causes brief recurrent seizures in the first days of life. More than 80% of SeLNE patients have a KCNQ2 or KCNQ3 mutation, which encode heteromers of a voltage-gated ion channel that serves to limit neuronal excitability.
One in four children with SeLNE develops epilepsy later in life. However, this risk is associated to the number of seizures in the neonatal period, suggesting the importance of early seizure control to optimize later outcomes. All patients reported in the 2016 study who received oral carbamazepine or oxcarbazepine stopped seizing after the first dose, whereas large intravenous loads with phenobarbital and levetiracetam were usually unsuccessful.
That paper together with subsequent publications of additional cohorts of newborns, led the International League Against Epilepsy to change their guidelines for SeLNE management, recommending practitioners to consider ion channel blockers for its treatment.
Genetic testing can also provide better prognostic information. "When we know the underlying cause of the condition, there's more information that we can give about the trajectory of the illness and its comorbidities," Dr. Sands noted. "Some of these conditions don't just affect the brain. The genes are expressed elsewhere, and there are other organ systems that may be involved."
Specialization in Pediatric Epilepsy
NewYork-Presbyterian is renowned for its expertise in epilepsy care in children as well as patients of all ages. There are Level 4 Comprehensive Epilepsy Centers, as designated by the National Association of Epilepsy Centers, at both NewYork-Presbyterian/Columbia and NewYork-Presbyterian/Weil Cornell Medicine. Additionally, NewYork-Presbyterian Morgan Stanley Children’s Hospital and NewYork-Presbyterian Komansky Children’s Hospital are major referral centers for children with hard-to-control seizures.
"Our epilepsy teams include experts in neurology, neurosurgery, and neuropsychology, all of whom are publishing research," Dr. Sands said. "We are able to bring all of these experts into a single room to debate what's best for each patient. We also collaborate with experts in neuroradiology and neuropathology. It's really a village."




