NewYork-Presbyterian has long been a leader in the development of laser ablation techniques to eliminate dysfunctional or diseased brain tissue. Building on that history, Brett Youngerman, MD, a neurosurgeon at NewYork-Presbyterian/Columbia, is actively exploring the efficacy of laser ablation in treating drug-resistant epilepsy.
“At NewYork-Presbyterian, we’re at the forefront of developing laser ablation techniques and technology, and we are one of the most experienced centers with laser ablation,” says Dr. Youngerman. “We're using that experience to constantly improve the technique, both by learning who are the best candidates for the procedure and how to best carry out the procedure technically.”
Patients with drug-resistant epilepsy have less than a three percent chance of seizure freedom with medications alone. This puts them at risk of significant morbidity and mortality that includes injuries and direct consequences of seizures, and long-term adverse effects on their mood, cognition, and psychological status. They are also at risk of Sudden Unexpected Death in Epilepsy (SUDEP).
At NewYork-Presbyterian, we’re at the forefront of developing laser ablation techniques and technology, and we are one of the most experienced centers with laser ablation. We're using that experience to constantly improve the technique, both by learning who are the best candidates for the procedure and how to best carry out the procedure technically.
— Dr. Brett Youngerman
All patients with drug-resistant epilepsy should be evaluated for surgery. The specific surgical intervention required depends on the location in the brain where the seizures originate. The most common location is the temporal lobe, where the gold standard treatment is anterior temporal lobectomy. Surgery offers a better chance of seizure freedom than medications alone and is generally well tolerated. Despite this, epilepsy surgery is underused.
“Surgical removal of the area of the brain that’s causing the seizures is actually very well tolerated, and it has a much better chance of seizure freedom,” says Dr. Youngerman. “Patients have improved cognitive function and quality of life after successful surgery. But for many patients, the idea of undergoing an open brain surgery and removal of part of the brain with surgery is still very unappealing and is a barrier to many patients considering a surgical procedure.”
Pursuing Alternatives to Open Surgery
Magnetic resonance image-guided laser interstitial thermal therapy (MRgLITT) is a minimally invasive alternative to open surgery. Unlike open surgery, this technique enables clinicians to access deep structures of the brain with minimal disruption to the overlying cortex and white matter. “We are actually able to ablate that area while the temperature is monitored in real time with the MRI,” says Dr. Youngerman. “We’re able to prevent overheating and minimize risk of injury to the surrounding structures while focusing on removing the area that we believe the seizures are originating from.”
This approach may appeal to patients as it is performed through a less than one-centimeter incision, is associated with minimal pain, and enables most patients to return home the next day. However, only small single-center studies had analyzed the seizure freedom rate with MRgLITT, reporting variable results, and long-term durability remained largely unknown.
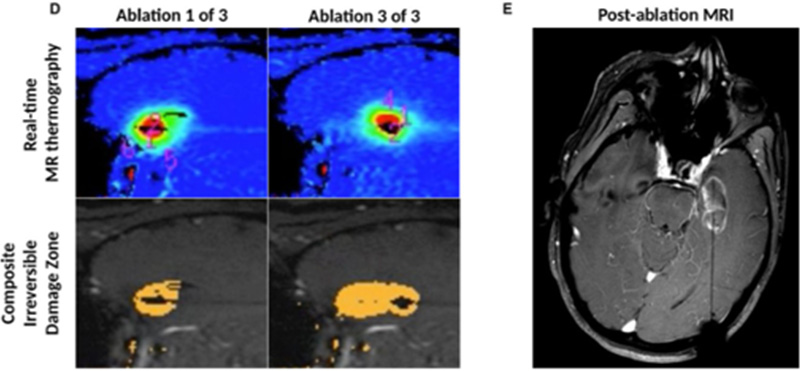
(L) MR thermography allows for monitoring of the ablation temperature to protect the surrounding critical structures from injury. Multiple ablations along the laser fiber trajectory allow for removal of the target areas. (R) A post-procedure MRI demonstrates the completed desired ablation of the epileptogenic focus.
Dr. Youngerman and his NewYork-Presbyterian/Columbia colleagues, including neurosurgeon Guy McKhann, MD, and neurologist Catherine Schevon, MD, PhD, recently completed a multicenter, retrospective cohort study to better understand the long-term outcomes of laser ablation therapy. The results were published in the Journal of Neurology, Neurosurgery, and Psychiatry. This study included 268 patients treated consecutively with mesial temporal MRgLITT at 11 centers, making it the largest study published to date.
The study found that, at a median follow-up of over four years, approximately half of the patients remained free of disabling seizures and about two-thirds of the patients had a favorable outcome defined as being free of disabling seizures or having rare disabling seizures. This study suggests that patients with specific findings on the preoperative workup may have better outcomes. These findings include the presence of mesial temporal sclerosis, concordant data, and seizures that didn’t generalize. The safety profile of MRgLITT was favorable compared to temporal lobectomy, with very few severe or permanent complications and most patients being discharged home the day after surgery.
Additionally, the study suggests that patients who do not successfully cure their seizures with first-line laser ablation therapy may still be candidates for open surgery with anterior temporal lobectomy. “We found that patients who choose laser ablation as a first line therapy may still be candidates for open surgery with an anterior temporal lobectomy if the laser ablation does not successfully cure their seizures,” says Dr. Youngerman. “Among the patients who continued to have seizures after a laser ablation and went on to anterior temporal lobectomy, about two thirds of these patients were still able to have freedom from disabling seizures, which is similar to what we see with patients undergoing upfront anterior temporal lobectomy.”
We found that patients who choose laser ablation as a first line therapy may still be candidates for open surgery with an anterior temporal lobectomy if the laser ablation does not successfully cure their seizures. Among the patients who continued to have seizures after a laser ablation and went on to anterior temporal lobectomy, about two thirds of these patients were still able to have freedom from disabling seizures, which is similar to what we see with patients undergoing upfront anterior temporal lobectomy.
— Dr. Brett Youngerman
Exploring Additional Uses of Minimally Invasive Techniques in Epilepsy
In addition to this study, Dr. Youngerman and his colleagues are looking at the effectiveness of laser ablation therapy for other types of drug-resistant epilepsy, such as hypothalamic hamartomas, cortical dysplasia, cavernous malformation, and low-grade epilepsy-associated tumors. Dr. Youngerman is also investigating the emerging field of neuromodulation for epilepsy. “When we find that seizures are coming from areas of the brain that can’t be safely removed, or we find that seizures are coming from multiple different areas of the brain and it would not be safe to remove those areas, then neuromodulation is an alternative option where we can try to stimulate to reduce seizures without having to remove any area of the brain. The field is evolving, and we understand that patients don’t want large open surgeries. We’re working to try and develop additional minimally invasive procedures that are more patient centered.”
The field is evolving, and we understand that patients don’t want large open surgeries. We’re working to try and develop additional minimally invasive procedures that are more patient centered.
— Dr. Brett Youngerman