For patients with ulcerative colitis, familial adenomatous polyposis, and other digestive conditions requiring the removal of the entire colon, the ileal pouch-anal anastomosis (IPAA or J-pouch), a surgical technique that creates an internal reservoir out of the small intestine to restore native bowel function, has become the preferred method of reconstruction following a total proctocolectomy. However, when a J-pouch fails or is not feasible, there is an alternative that has historically been underutilized but can be equally as effective: the continent ileostomy (CI), also known as the Kock pouch or K-pouch.
The CI involves removal of the colon and creation of an internal reservoir for waste elimination. It differs from the traditional end ileostomy in that it does not require an external ostomy appliance to catch waste. It also differs from the J-pouch because it allows patients to empty their appliance through the catheterization of a discreet stoma rather than defecation through the anus.
Ravi P. Kiran, M.D., a colorectal surgeon and co-director of the Global Center for Integrated Colorectal Surgery and IBD Interventional Endoscopy at NewYork-Presbyterian and Columbia, is one of a handful of surgeons in the world who performs this procedure regularly. He and his colleagues recently published a decade-long retrospective study that underscores the procedure’s durability, safety, and patient satisfaction.
“There are many advantages to the continent ileostomy,” says Dr. Kiran. “It can improve cosmetic appearance, allow for better activity and exercise, address skin problems, and potentially improve nutrient absorption compared to standard ileostomies. We have seen very good outcomes for patients who report a good quality of life.”
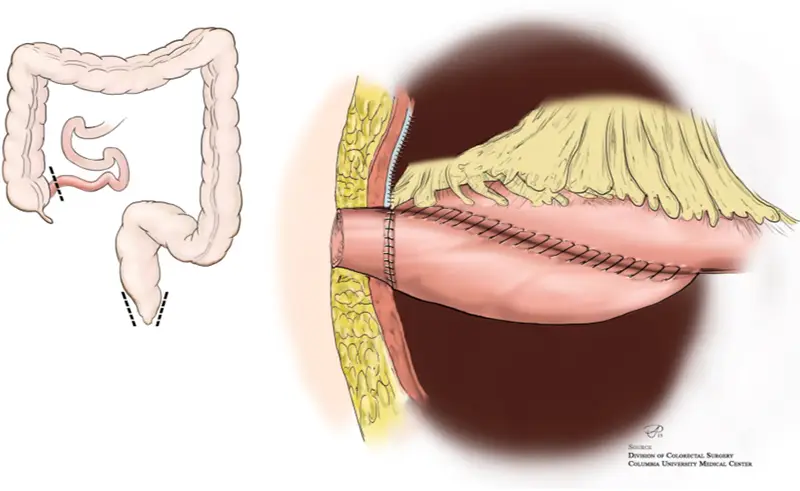
In a continent ileostomy, the colon is removed and an internal reservoir is created out of the small intestine and attached to a stoma in the abdomen. Waste can then be removed by the patient via catheter. Illustration courtesy of the Division of Colorectal Surgery at Columbia.
Reassessing the Role of the Continent Ileostomy
First introduced in 1967 by Dr. Nils Kock, the K-pouch procedure was originally created to address patients’ dissatisfaction with uncontrolled passage of stool through an end ileostomy.
Its use declined over the years following the rise of the J-pouch, largely due to CI surgery’s technical complexity and high early revision rates. But Dr. Kiran and his colleagues in the Pouch Salvage and Continent Ileostomy Program in the Global Center for Integrated Colorectal Surgery and IBD Interventional Endoscopy have demonstrated that, with appropriate surgical training and multidisciplinary support, CI can achieve excellent outcomes even in newly created pouches.
In their recent paper, Dr. Kiran and his colleagues reported on their 10-year retrospective experience performing the procedure at NewYork-Presbyterian and Columbia. Their goals were to examine the current role of CI in colorectal surgery, report on outcomes of CI surgeries in the present era, and detail the creation of a pouch program at an academic medical center.
The researchers examined the outcomes from 95 CI procedures performed on 80 patients from 2013 to 2023, including 38 new pouch creations, 52 CI revisions, and five pouch excisions. The short-term outcomes were promising:
- Mean hospital stay: 8.4 days
- 30-day readmission rate: 29%
- Major complication rate (leak or pelvic abscess): 11%
- No postoperative mortality
Eighty-seven percent of patients retained their CI after an average of 37 months of follow-up. Pouch revision was required in 34% of patients, with common causes including slipped nipple valve, exit conduit stenosis, parastomal hernia, and pouch fistula.
Importantly, 92% of patients in the new pouch group and 93% in the revision group reported improvements in function and quality of life: 96% even stated they would recommend the procedure to others. “Even in this day and age, we have very good CI outcomes and our patients are very happy,” says Dr. Kiran. “If you look at their quality of life and happiness, the data supports that CI is a good option to be offered to patients.”
Patient and Surgical Considerations
Not everyone is a candidate for this procedure. Dr. Kiran notes that ideal candidates for CI include:
- Patients with J-pouch failure
- Patients unable to tolerate external ostomy appliances
- Patients with significant peristomal skin issues
- Patients with pelvic floor dysfunction or impaired continence
Patients who opt to undergo the procedure must also have adequate small bowel length and healthy bowel tissue, as approximately 60 centimeters of small intestine is used in the creation of the pouch and valve. CI is contraindicated in patients with active Crohn’s disease involving the small intestine, due to the risk of disease recurrence and the potential need for additional bowel resection.
“It’s essential that both the patient and surgeon are motivated, as this is a complex procedure,” says Dr. Kiran. “The surgical team must understand the nuances of managing the CI postoperatively and be able to hold the hands of patients through potential issues that can occur.”
The surgery itself demands high technical skill, particularly in the construction of the intussuscepted nipple valve — a key component for maintaining continence. Dr. Kiran has refined the technique using topical doxycycline to promote serosal adhesion and minimize valve slippage, one of the most common reasons for revision. His team reports a valve slip rate of 16%, consistent with or better than historical norms.
This surgery should not be a relic of the past. We should be thinking of it as a forward-looking option for the right patient, in the right hands.
— Dr. Ravi Kiran
A Call for K-pouch Reconsideration
In the context of the growing population of complex IBD patients — including those presenting after failed medical management, J-pouch failure, and pelvic floor dysfunction — the need for alternative reconstructive options is more pressing than ever. The CI offers one such option, particularly for motivated patients who can handle the learning curve associated with pouch care. “This surgery should not be a relic of the past,” Dr. Kiran says. “We should be thinking of it as a forward-looking option for the right patient, in the right hands.”
As the surgical community seeks to expand personalized treatment options for patients undergoing proctocolectomy, Dr. Kiran calls for the continent ileostomy to receive renewed consideration and for more awareness and training among gastroenterologists and colorectal surgeons. “Many providers simply don’t offer it because they’re not aware it exists or they don’t believe it works,” Dr. Kiran says. “But when done well, patients are overwhelmingly satisfied and grateful for the improved quality of life it offers.”




