Dr. Jeffrey Geller
“As we look back on all the years and all of the technological advancements in knee replacement surgery, including computer navigation and robotics, there remains close to a 15 to 20 percent dissatisfaction rate,” says Jeffrey A. Geller, MD, Chief, Division of Hip and Knee Reconstruction and Director of Research, Center for Hip and Knee Replacement, at NewYork-Presbyterian/
While femoral component rotation has undergone rigorous research, with the largest study published by the NewYork-Presbyterian/
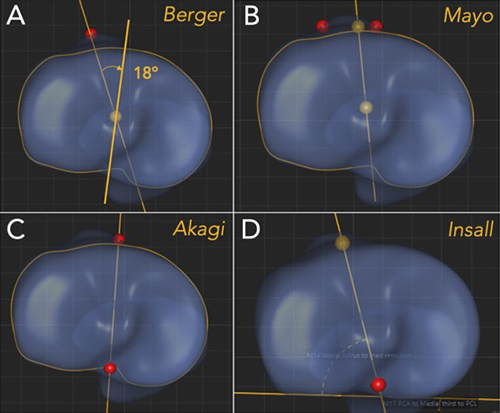
Tibial tubercle-based reference axes for tibial rotation (Courtesy of Dr. Jeffrey Geller)
Dr. H. John Cooper
“At Columbia, we were interested in examining some of the intraoperative decisions that we make when doing knee replacements,” adds H. John Cooper, MD, another orthopedic surgeon at NewYork-Presbyterian/
“Surgeons have many ways of determining the optimal placement of the components. For any implant placed in the body, considerations need to be made based on the three-dimensional orientation,” notes Dr. Geller. “While there are many theories and a variety of smaller research studies examining the ideal placement of components when performing a total knee replacement, we believe our studies are the first large-scale projects to specifically identify anatomic landmarks, thereby providing a scientific foundation behind how to best place these implants rotationally.”
While there are many theories and a variety of smaller research studies examining the ideal placement of components when performing a total knee replacement, we believe our studies are the first large-scale projects to specifically identify anatomic landmarks, thereby providing a scientific foundation behind how to best place these implants rotationally.— Dr. Jeffrey Geller
The current study on tibial component rotation by Dr. Geller, Dr. Cooper, along with Roshan P. Shah, MD, JD, Director, Complex Adult Hip and Knee Reconstruction at Columbia, sought to examine proposed methods that support the surgeon’s intraoperative judgment in determining which method is the most reproducible for ideal rotational placement and identify the landmarks that can improve that placement. There are some eight or nine different ways of rotating the tibia that have been described in the literature. To narrow the field, the Columbia researchers reviewed nearly 1,400 CT scans of the entire tibia from the SOMA (Stryker Orthopaedic Modeling and Analytics) database.
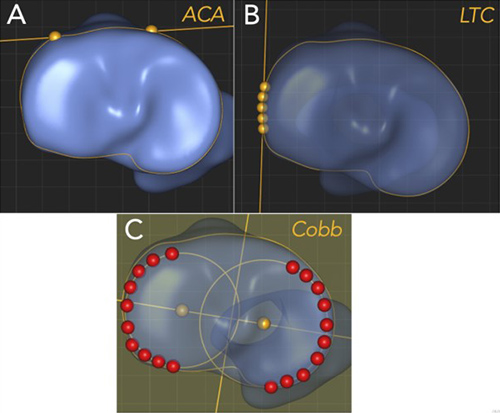
Non-tubercle-based, intra-articular reference axes for tibial rotation (Courtesy of Dr. Jeffrey Geller)
“The three of us have been working together for some time and are the senior hip and knee replacement surgeons within the Department of Orthopedic Surgery,” notes Dr. Geller. “Dr. Eugene Jang is a former Columbia orthopedic surgery resident, who had an engineering background before going to medical school. He came to us and suggested the study. We agreed that the topic was important and together we formed the research team with Dr. Jang as lead author.”
The results of their study, which were published in the January 4, 2023, issue of The Journal of Bone & Joint Surgery, revealed the following:
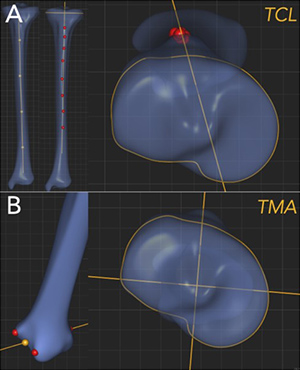
Extra-articular, distal reference axes for tibial rotation (Courtesy of Dr. Jeffrey Geller)
- The Mayo method and the Insall line both offer an ideal balance of accuracy, low variability, and a reduced likelihood of internal rotation errors.
[The Mayo method involves a line connecting the medial and middle one-thirds of the tibial tubercle and the geometric center of the tibia; the Insall line involves a line connecting the posterior cruciate ligament insertion and the intersection of the middle and medial one-thirds of the tibial tubercle.] - No clinically significant gender-based or ethnicity differences were found, with the exception of consistently greater tibial intorsion in Asian versus Caucasian individuals.
- The rotational axes based on landmarks farther from the knee were less reliable than those based on intra-articular landmarks; setting rotation on the basis of distal landmarks, such as the tibial crest line and transmalleolar axis, may predispose surgeons to substantial malrotation errors, especially given the differences in tibial torsion found between ethnic groups.
This is the first study to compare all of the described methods of determining tibial rotation to identify which one would be most reproducible for surgeons to use intraoperatively.— Dr. H. John Cooper
Two Schools of Thought on the Tibial Component
“The study provided objective, radiographic-based evidence to optimally reproduce the native anatomy, keeping in mind that subjectivity likely will never be fully eliminated,” says Dr. Geller.
“There are two main schools of thought on placing the tibial component during surgery – anatomic and kinematic. The anatomic approach for tibial component rotation is based on reproducible anatomic landmarks regardless of the deformity or degree of arthritic changes. The tibial baseplate is always placed with the anterior aspect of the middle of the component lining up with the junction of the medial and middle thirds of the tibial tubercle. This was how I was trained, and it continues to be my personal choice of method and the one I use in training residents and fellows.”
In contrast, rotational alignment of the tibial tray with the kinematic approach is predicated on the tibial trial component engaging with the femoral component while the knee is put through flexion-extension cycles. “The femoral component, which is placed first with the tibial baseplate floating on the top of the tibia, then dictates the rotation of the tibia and where it is placed. This presents a fair amount of variability,” explains Dr. Geller. “Supporters of this method believe that because everyone’s knees wear out differently and have a different muscle and ligament slope that conforming placement of the tibial baseplate to the femoral component will achieve a better soft tissue balance and a closer replication of native joint biomechanics.”
Dr. Geller believes that with the kinematic approach if close attention is not paid to the rotation of the tibial baseplate relative to anatomic landmarks, then there is a risk for a poor outcome. “Our study data provides additional guidance on placing the tibial baseplate. There are many factors that go into a successful knee replacement, and there is little room for error before a replacement does not provide the optimal pain relief patients are seeking. This is the first study that ties together several factors that can serve as a practical guide for orthopedic surgeons.”
Dr. Cooper concurs. "The optimal way to rotate the tibial component in that third dimension is an area that was less clear before this study. We’re now giving surgeons an easy-to-identify landmark that can allow them to rotate the tibial component appropriately and maximize the chances of a successful placement. By leveraging a large 3D database, we were able to draw conclusions that could not have been made in smaller studies.”
“There are a number of landmarks that we see when doing a knee replacement that we may or may not choose to utilize when trying to determine the optimal rotation of the tibial component,” continues Dr. Cooper. “The landmark that we identified as being the most reproducible with the least chance or error is the junction of the medial and middle third of the tibial tubercle, which we see in every total knee replacement surgery.”
“This is an important study with the potential to decrease the incidence of patient dissatisfaction after knee replacement surgery,” says Dr. Geller. “Malrotation of components and the tibial baseplate are among the most common reasons I see in patients needing revision knee replacement. I encourage surgeons to pay attention to a study like this and incorporate it into their workflow and their surgical technique because it can help improve patient outcomes.”