A Breath of Life
A rare EXIT procedure gave a newborn a fighting chance.
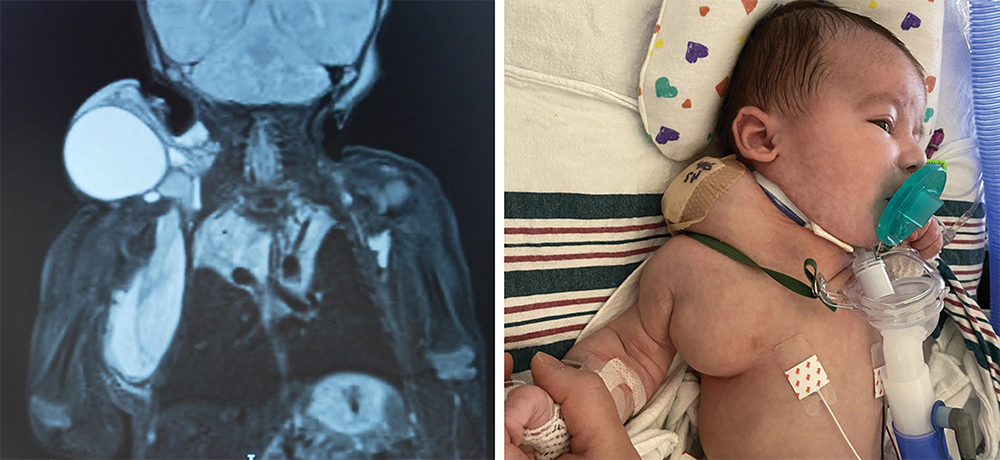
When Ashley and Mark Merchant Learned Their Unborn Baby’s Airway Was Threatened by a Large and Complex Lymphatic Malformation, they were told to prepare for the worst. Living in Maine, they had scant options for lifesaving intervention; their search quickly took them to experts at NewYork-Presbyterian/Weill Cornell Medical Center for their only hope in giving their baby a chance to survive outside the womb.
At Ashley’s first visit, maternal-fetal medicine specialist Dr. Julianne Lauring confirmed the dire diagnosis: A mass extended through the baby’s neck and throat, blocking his airway. Ashley “told me to do anything we could to give her baby a chance,” Dr. Lauring recalls. That commitment set in motion one of the most complex and coordinated procedures NewYork-Presbyterian performs: an EXIT procedure, or ex utero intrapartum treatment, a rare and high-risk operation in which a baby is partially delivered by C-section but remains connected to the placenta while surgeons secure the airway.
“The procedure carries risk for both mother and baby,” says Dr. Lauring. “But at NewYork-Presbyterian, we have the expertise, the infrastructure, and the collaborative culture to do it safely.”
Over several months, Dr. Lauring convened a multidisciplinary team that included obstetric and pediatric anesthesiologists, neonatologists, pediatric otolaryngologist Dr. Steven Rosenblatt, interventional radiologist Dr. Bradley Pua, and specialized nurses. Together, they held simulations to choreograph every movement in the operating room. “That’s what makes NewYork-Presbyterian unique,” says Dr. Lauring. “We have every subspecialist under one roof, all working together for a single patient.”
When Ashley was 35 weeks pregnant, more than 40 specialists gathered in the OR for the EXIT procedure. “You have roughly 30 minutes to secure the airway before the baby loses oxygen,” says Dr. Rosenblatt. Using advanced endoscopic tools, he visualized the larynx and successfully intubated the newborn while he was still attached to the placenta. “I called out, ‘I have the airway,’ and everyone cheered,” he says. Finnley was then safely delivered, a success that depended on the seamless collaboration of multiple teams.
After birth, Finnley underwent additional procedures to shrink the mass obstructing his airway. Drs. Pua and Rosenblatt worked together to perform minimally invasive sclerotherapy, an advanced technique available only at centers with highly specialized expertise. “The area we needed to access was deep in the neck, surrounded by critical structures,” says Dr. Rosenblatt. “It required complementary skill sets and absolute trust.”
Four months later, Finnley was home, thriving, and meeting his milestones. “Our NewYork-Presbyterian care team never gave up,” says Ashley. “No matter what challenge came up, they found the exact right care every time.”
