Major Grant Propels Research in Early Stage Parkinson’s Disease
Weill Cornell Medicine neuroscience investigators have received a major funding boost of nearly $9 million from the Align Science Across Parkinson’s (ASAP) initiative that focuses on early-stage Parkinson’s disease. ASAP is a coordinated research collaborative emphasizing open science and is committed to advancing targeted basic research that will accelerate the pace of discovery and inform the path to a cure. The Michael J. Fox Foundation for Parkinson’s Research is ASAP’s implementation partner and issued the grant.
Neurosurgeon Michael G. Kaplitt, MD, PhD, Vice Chairman for Research in the Department of Neurological Surgery and Director of Stereotactic and Functional Neurosurgery at NewYork-Presbyterian/Weill Cornell Medical Center, leads an ambitious multi-institutional effort studying how abnormal protein aggregates may spread from the gut to the brain to drive the early stages of Parkinson’s disease.
Dr. Michael Kaplitt
“Interaction between the body and the brain is a very exciting and important area of research, and it is increasingly clear that, at least in some cases, Parkinson’s disease may begin in the gut, with the disease spreading through nerve connections to the brain and eventually throughout the brain,” says Dr. Kaplitt, an internationally recognized pioneer in innovative treatments for brain and nervous system disorders.
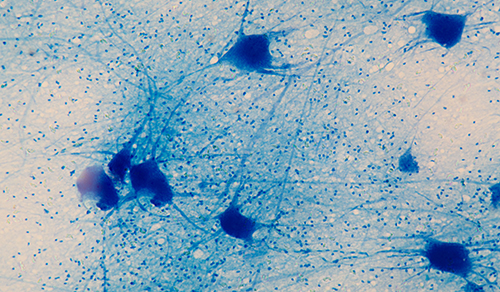
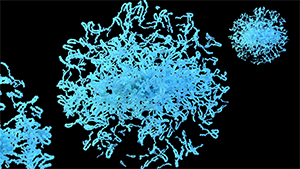
One clue to the cause of Parkinson’s disease is the presence of abnormal clumps of protein within brain cells in affected brain regions. These clumps mainly consist of tiny, fiber-like aggregates of the brain-cell protein alpha synuclein. The synuclein fibrils tend to spread through the brain in a characteristic pattern during the course of Parkinson’s. Evidence suggests that in many cases these disease-linked fibrils form initially in nerve cells in the intestines and trigger the classic signs of Parkinson’s only after they travel to the brain via the vagus nerve.
Alpha synuclein protein aggregate
Dr. Kaplitt and his collaborators will use a mouse model of this gut-to-brain disease-seeding process to explore how it begins in the intestines; how it relates to early, “pre-motor” Parkinson’s signs, including sleep disorders; and whether it differs between males – who are prone to Parkinson’s at a higher rate – and premenopausal females. Ultimately the researchers will try to develop methods for the early detection of gut alpha-synuclein aggregates and the blocking of their spread to the brain to prevent full-blown Parkinson’s.
Dr. Kaplitt’s team includes faculty from the Meinig School of Biomedical Engineering at Cornell University, who will employ novel methods they have developed to image vagus-linked gut neurons to track the spread and the physiological effects of early synuclein pathology.
Dr. Babacar Cisse
Dr. Roberta Marongiu
In addition, Babacar Cisse, MD, PhD, a neurosurgeon with NewYork-Presbyterian/Weill Cornell Medical Center and an expert in the immune cells in the brain called microglia, will investigate whether microglia are responsible for some of the patterns of spread once the pathology enters the brain from the gut.
Roberta Marongiu, PhD, Assistant Professor of Neuroscience Research in Neurological Surgery in the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine, will study how sex and menopause influence the spread of Parkinson’s disease pathology from the gut to the brain. “This will help us understand more about the intricate relationship between hormones and onset of Parkinson’s disease and has the potential to identify novel precision medicine approaches for men and women,” says Dr. Marongiu, Co-investigator.
“Our nearly 30 years of experience with gene therapy, beginning with the first human Parkinson’s gene therapy treatment at NewYork-Presbyterian/
Weill Cornell Medical Center and continuing with several active trials today, will allow us to not only understand how this gut-to-brain transmission happens, but also potentially intervene genetically to improve brain function and stop the spread of disease.” — Dr. Michael Kaplitt
Collaborators on the research also include co-investigators Ted M. Dawson, MD, PhD, Director of the Johns Hopkins Institute for Cell Engineering and Professor of Neurology at the Johns Hopkins University School of Medicine, and Per Svenningsson, MD, PhD, Professor of Neurology at Karolinska Institutet and Karolinska University Hospital in Sweden.
“Bringing together this international team of the most forward-thinking, most innovative researchers in Parkinson's disease holds so much promise for patients,” says Philip E. Stieg, PhD, MD, Chair of Neurological Surgery at Weill Cornell Medicine and Neurosurgeon-in-Chief of NewYork-Presbyterian/Weill Cornell Medical Center. “We all look forward to the discoveries that come from this research, which has the potential to create effective new treatments for this debilitating disease."
Related Publications