Perspectives in Bariatric Metabolic Surgery
Dr. Marc Bessler
The field of bariatric metabolic surgery continues to evolve as new procedures emerge demonstrating improved risk and benefits. At the Center for Metabolic and Weight Loss Surgery at NewYork-Presbyterian/Columbia University Irving Medical Center, under the direction of Marc Bessler, MD, surgeons are pioneering weight loss techniques and continue to refine minimally invasive approaches to advance the field.
Sleeve Gastrectomy versus Roux-en-Y
Metabolic problems associated with obesity have been a primary focus of bariatric surgeons for years and, in the last decade, the understanding of how surgical interventions can favorably alter metabolism has increased, notes Dr. Bessler, who is also Chief of the Division of Minimal Access/Bariatric Surgery, and Director, Minimal Access Surgery Center. “In general, weight loss surgery can achieve diabetes remission, but the Roux-en-Y gastric bypass and duodenal switch have been shown to be the most effective procedures for diabetes control.”
Dr. Bessler and his colleagues collaborate with endocrinologists on clinical initiatives, as well as studies seeking to improve outcomes of patients challenged by obesity. They were among the first to characterize the role of hormonal changes from the gut, especially the PYY effect, and they continue to actively study the duration of these effects and other outcome-related factors. They have demonstrated in research studies that the anti-diabetes effect of certain bariatric procedures – particularly gastric bypass surgery – results from mechanisms that go beyond weight loss, supporting the use of this approach for treating type 2 diabetes.
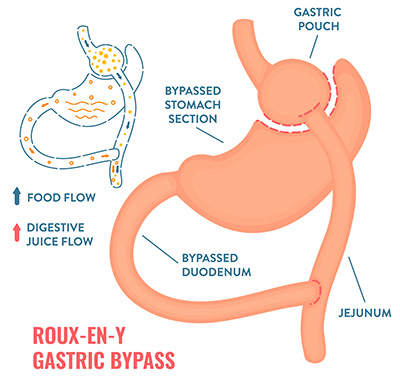
Illustration of Roux-en-Y gastric bypass
In a study published in the February 2019 issue of Science Reports, they compared sleeve gastrectomy, which is growing in favor today, with Roux-en-Y gastric bypass. “Some randomized trials have shown lower weight loss and HbA1c improvement with sleeve gastrectomy compared with gastric bypass,” says Dr. Bessler. “Our study objective was to compare changes in beta-cell function following both procedures in patients who are obese and have type 2 diabetes with similar weight loss.”
Patients undergoing sleeve gastrectomy were studied with an intravenous glucose tolerance test before surgery and at 5 to 12 percent weight loss post-surgery. “We concluded that both sleeve gastrectomy and gastric bypass improve beta-cell function in the short term in obese patients with type 2 diabetes when assessed using an IV glucose challenge,” says Dr. Bessler. “However, further studies are needed to determine if longer-term clinical outcomes tend to be better after gastric bypass due to greater weight loss and/or other factors that differ between the procedures as a consequence of the different anatomical alterations.”
In a study published in the July 20, 2020 issue of PLOS ONE, the Columbia research team investigated the differences in the effect of sleeve gastrectomy and Roux-en-Y gastric bypass on gastrointestinal hormones that regulate energy homeostasis. Their focus was on the roles of PYY, glucagon-like peptide-1 (GLP-1), and ghrelin for regulating glucose homeostasis and energy balance. By prospectively quantifying blood levels of gut hormones of energy and glucose homeostasis at one-year follow-up, they demonstrated significant changes after bariatric surgery in levels of the gut hormones that regulate glucose and energy homeostasis. Increases in postprandial PYY and GLP-1 levels in the blood were observed primarily after the Roux-en-Y procedure and transiently after sleeve gastrectomy.
The researchers concluded that differences in gastrointestinal hormones of energy homeostasis and changes in sweet cravings are possible mechanisms for greater weight loss and may mediate weight-independent improvement in insulin resistance after Roux-en-Y gastric bypass.
Read more:
Arakawa R, Febres G, Cheng B, Krikhely A, Bessler M, Korner J. Prospective study of gut hormone and metabolic changes after laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. PLOS ONE. 2020 Jul 20;15(7):e0236133.
Mullally JA, Febres GJ, Bessler M, Korner J. Sleeve gastrectomy and Roux-en-Y gastric bypass achieve similar early improvements in beta-cell function in obese patients with type 2 diabetes. Scientific Reports. 2019 Feb 12;9(1):1880.
Loop DS: A Variation of the Duodenal Switch
“The duodenal switch is basically a sleeve gastrectomy plus intestinal bypass,” says Dr. Bessler. “By shortening the area of the intestine where food is absorbed, this approach more rapidly stimulates the satiety hormones that are released from the intestines. The duodenal switch gives patients the advantage of a sleeve gastrectomy by eliminating ghrelin, but also adding the satiety hormones, PYY and GLP-1. Most patients can expect to lose 60 percent of their excess body weight with sleeve gastrectomy, 70 percent with gastric bypass, and closer to 80 percent with the duodenal switch. A duodenal switch is the most effective for both weight loss and diabetes resolution.”
“A duodenal switch is the most effective approach for both weight loss and diabetes resolution.” — Dr. Marc Bessler
Dr. Bessler and his Columbia colleagues also perform a variation of the classic duodenal switch with the single anastomosis duodenal ileostomy or loop DS. “The risk of leaking and spilling potentially harmful matter into the peritoneum is significantly increased with every anastomosis,” continues Dr. Bessler. “Additionally, fewer connections directly translate into a possibly shorter surgery, making it easier to perform in one step and reducing intraoperative risks such as hemorrhage and infection. In the loop DS, we attach the small intestine to the duodenum just below the stomach. It seems to be as effective, certainly for weight loss, and with less weight regained over time.”
Dr. Bessler notes that the loop DS is often used as a revision technique for patients gaining back their weight after sleeve gastrectomy. “Unless they have acid reflux, we would go back to taking the sleeve and adding the intestinal component, either a loop or the duodenal switch. More frequently today we would offer the loop.”