Mitral Valve Disease: Maximizing Outcomes with Teamwork and New Technology
The first successful mitral valve repair was performed in 1923 under emergency duress on a comatose young girl with rheumatic mitral valve stenosis. This initial triumph led the surgeon to attempt to develop a protocol for operating on faulty mitral valves. He set his project aside when he was unable to reproduce his initial surgical success on other forms of mitral valve dysfunction. It would be more than another three decades before the first successful mitral valve repair for insufficiency would take place.
Now, in an era of extraordinary developments in research and technology that are able to be rapidly applied to cardiac care, less invasive treatments for mitral valve disease are coming on board at an astonishing pace — many pioneered, evaluated, or refined by the heart teams at NewYork-Presbyterian. Cardiologists, interventional cardiologists, and cardiac surgeons at NewYork-Presbyterian/Columbia University Irving Medical Center and NewYork-Presbyterian/Weill Cornell Medical Center bring their expertise to bear in collaborations that cross disciplines and support unprecedented progress within programs that allow the details of the patient’s disease to dictate the best treatment.
Contemporary treatment of mitral valve disease is multidisciplinary and may involve medical therapies, surgical treatments, and most recently, catheter-based procedures. Patients who come to NewYork-Presbyterian benefit from a comprehensive evaluation by multidisciplinary heart teams, which will make the determination of the appropriate therapeutic option based on several factors, including the severity of symptoms, operative risk, and comorbidities.
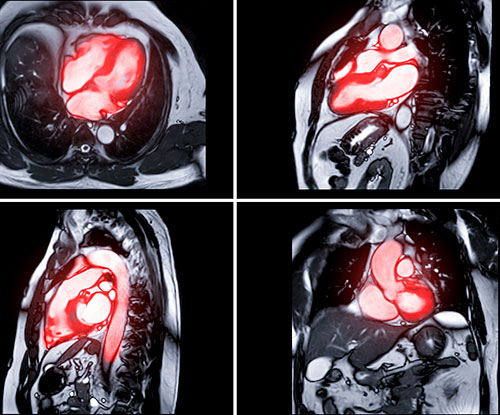
Magnetic resonance imaging used for the diagnosis of heart disease
Mitral valve disease is not a trivial issue in terms of its prevalence. Mitral regurgitation (MR) is the second most common valvular heart disease in the Western world with a prevalence in the United States alone of two to four million people. Nearly one in 10 people age 75 and older has moderate or severe MR. Sternotomy has served as a barrier to surgery for many of those with mitral valve disease and other valvular disorders, setting the stage for the development of new approaches to replace or repair the mitral valve without disrupting the important structures that are attached to the valve itself.
Over the past five years, our cardiac surgeons have performed more than 500 mitral valve surgical procedures annually. During this time, our cardiac surgeons have also transitioned their operative approach from replacement to repair and from open surgery to minimal access methods— including less invasive mini-thoracotomy, keyhole, and robotic procedures — with great success.
With increasing evidence that mitral valve repair has superior outcomes to replacement, the surgical treatment of mitral valve disease, particularly for mitral valve prolapse, is becoming more of a specialty operation best performed at high-volume academic medical centers such as NewYork-Presbyterian.
Exploring and implementing these newer approaches to treat mitral valve disease less invasively is an institution model for NewYork-Presbyterian, where cardiac patients are at the uppermost level of surgical risk and complexity, and where our mortality rates, at about one percent, are among the lowest nationally.
Mitral Valve Treatment Today
The variety of advances now being studied and tested in the treatment of mitral valve disease are providing patients with more choice and permitting those who would have been excluded from treatment— the elderly or critically ill — the opportunity for meaningful therapy.
Exploring and implementing newer approaches to treat mitral valve disease less invasively is an institution model for NewYork-Presbyterian, where cardiac patients are at the uppermost level of surgical risk and complexity, and where our mortality rates, at about one percent, are among the lowest nationally.
Minimally Invasive Surgery
Mini-Thoracotomy Surgeons at NewYork-Presbyterian have been performing minimally invasive mitral valve surgery since 1998 and participated in the first clinical trials of robotic mitral valve repair over 15 years ago. The most common minimally invasive approach performed by our surgeons is a right mini-thoracotomy, which utilizes a three- to four-inch incision between the ribs without cutting the breastbone, and allows mitral valve repair or replacement, as well as associated procedures, such as tricuspid valve repair, atrial septal defect repair, and the Maze procedure for atrial fibrillation. To date, our surgeons have performed over 1,500 mitral valve operations via this minimally invasive approach and have taught this technique to hundreds of surgeons from all over the world.
The Robotic Approach NewYork-Presbyterian’s cardiac robotic surgery program, one of the few in the country, continues to grow under the direction of a cardiac surgeon with more than 15 years of experience in performing, evaluating, and refining a wide range of totally robotic cardiac surgical procedures. The program incorporates the latest iteration of robotics technology — da Vinci Xi® — for mitral valve reconstructions. While the earlier versions of the da Vinci robot involved a fairly large incision, the current procedure utilizes four 8 mm ports. The da Vinci Xi surgical system employs instruments that are as dexterous as a surgeon’s hands, but considerably smaller, and a 3-D camera that provides vividly clear visuals. The minimally invasive approach, which is performed through small incisions on the right side of the chest, produces shorter hospitalizations of two to three days and less morbidity postoperatively.
Our cardiothoracic surgeons are now routinely performing endoscopic robotic surgery repair, particularly for patients with mitral valve regurgitation. The procedure is performed through four 8 mm incisions and one 12 mm incision — considered the smallest incisions used for this procedure in the nation.
A major advantage of endoscopic robotic surgery over traditional sternotomy, non-robotic, or robotic port access approaches is that rib spreading is not needed. In addition, approaching the valve robotically from the right side of the chest allows the valve and the heart to remain in their natural positions rather than having to retract the heart to expose the valve. A catheter-based system is used to place the patient on the heart-lung machine, which enables the surgery to be accomplished completely through the minute ports. The endoscopic approach also allows the surgeon to visualize the valve in its natural position, greatly facilitating the repair and resulting in a very high repair rate.
Considered the least invasive approach of the mitral valve procedures, robotic surgery is typically found to be most beneficial in distant, small cavities or contained areas, such as the left atrium where the mitral valve sits. The robot excels in these situations, making it possible to take the camera into that small space and have the same degree of freedom as if the surgeon’s hands were physically in that space.
MitraClip®
Patients with significant symptomatic degenerative mitral regurgitation who are not candidates for surgery are benefitting from the FDA-approved MitraClip, a low-risk, catheter-based procedure that creates a tissue bridge between the anterior and posterior leaflets using one or two clips that are deployed through a transseptal approach. The procedure is performed on a beating heart utilizing echocardiography for guidance. There are no major incisions and the recovery is essentially immediate, with patients able to go home the same or next day.
The MitraClip, which is now available for high-risk patients with degenerative mitral valve disease, continued under evaluation in the Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation (COAPT) multicenter trial, for which a NewYork-Presbyterian faculty member (Gregg W. Stone, MD) serves as one of the four national Principal Investigators. The COAPT trial recently completed enrollment of approximately 610 patients, with results anticipated later this year.

MitraClip therapy has become a well-established transcatheter approach for mitral valve disease.(Courtesy of Abbott)
The Transcatheter Approach
The consensus among NewYork-Presbyterian’s mitral valve team members is that the next quantum advancement in the treatment of mitral valve disease is going to be in percutaneous mitral valve replacement and repair, essentially the mitral version of TAVR. Over the past several years, there has been dramatic progress in terms of device technologies and patient selection for TAVR, based partly on the transformative work of interventional cardiologists and cardiac surgeons at NewYork-Presbyterian. Over the next five years, we expect the same transformative moment for transcatheter options for mitral valve disease. Our physicians have served and continue to serve as Principal Investigators in landmark trials related to transcatheter valve therapies, which now include multicenter studies for mitral valve disease.
NewYork-Presbyterian faculty served as lead investigators (Vinayak N. Bapat, MD, and Martin B. Leon, MD) in an international, multicenter study on early experience with a new transcatheter mitral valve replacement (TMVR) prosthesis. The results of the Intrepid TMVR Pilot Study were reported in the January 2, 2018, issue of the Journal of the American College of Cardiology. In an evaluation of 50 patients from 13 sites, the study found that the new valve represents a feasible minimally invasive alternative to surgical mitral valve replacement in patients with symptomatic MR who were deemed at high or extreme risk by the local heart teams.
| TMVR Pilot Study – Outcomes at 30 Days | |
|---|---|
| Device implant success | 98% |
| Device malfunction or thrombosis | 0 |
| 30-day mortality | 14% |
| Symptom improvement in follow-up | 79% |
The authors reported that “the Intrepid TMVR System is easy to implant in the challenging mitral anatomy due to its conformable, dual stent design.” The system integrates self-expanding, dual-stent technology with a tissue valve to facilitate catheter-based implantation without the need for open heart surgery. The device was shown to correct the underlying mitral regurgitation in a significant majority of patients.
NewYork-Presbyterian cardiac teams are also working closely with engineers to refine these devices and their delivery systems to make them as least invasive as possible. Currently, they have three iterations under development and testing:
- decreasing the bulk of the replacement valves
- creating the capability of completely withdrawing the device that was implanted and inserting another implant and repositioning it, if needed
- reducing the size of the delivery system from 1 or 1.2 cm to 8 mm diameter, enabling the device to be delivered through the groin without opening the chest
In addition to transcatheter mitral valve replacement, physicians at NewYork-Presbyterian are helping to lead trials utilizing novel devices to repair rather than replace damaged mitral valves. One such device is the Edwards Cardioband System, which allows physicians to place a ring around the mitral valve via the femoral vein without any incisions. This ring can be cinched down to reduce the mitral annulus (supporting structure for the mitral valve) and reduce mitral regurgitation. The procedure mimics the surgical annuloplasty ring but avoids any incisions. This device is currently being studied in a feasibility trial for patients with symptomatic, severe functional mitral regurgitation.
Valve-in-Valve Procedures

SAPIEN 3 is the only valve approved for mitral valve-in-valve procedures. (Courtesy of Edwards Lifesciences)
In June 2017, the FDA approved aortic and mitral valve-in-valve procedures using the Edwards Lifesciences SAPIEN 3 transcatheter heart valve. NewYork-Presbyterian physicians were involved in much of the initial research for the SAPIEN 3 valve, which is the first transcatheter heart valve approved in the U.S. for both aortic and mitral patients who are at high risk for a subsequent open heart surgery to replace their bioprosthetic valve.
The FDA stated that the SAPIEN 3 valve should only be used in patients who are at high or greater risk of death or serious complications from traditional open heart surgery to replace the failed surgical tissue valve.
Related Publications