Quality & Patient Safety Initiatives
The Department of Orthopedic Surgery at NewYork-Presbyterian/Columbia University Irving Medical Center continued with comprehensive efforts to improve quality and safety for orthopedic care of patients under the leadership of Michael G. Vitale, MD, MPH, Vice Chief of Quality and Strategy, and Kevin Wang, MHA, Director of Quality and Value. In the past four years since the inception of a formal quality and patient safety program, the Department has broadened its focus immeasurably and now includes:
Alternative Payment Models
Spearheaded by Kevin Wang, novel pay-for-performance strategies are being explored with payers, who are interested in investing in Columbia as a result of data that demonstrate the excellence of processes implemented by the Department and the outstanding outcomes of our orthopedic specialists.
Best Practices for Spine Care
Our orthopedic surgeons are working in collaboration with five other hospitals and MCIC Vermont, an insurance company for NewYork-Presbyterian and Columbia, to develop best practices in spine care with a goal to decrease complications and liability.
Surgical Site Infections
The Department continues at the forefront in the development of novel strategies and best practices for decreasing surgical site infections related to spine and total joint procedures. Since the quality team began monitoring antibiotic prophylaxis in 2015, compliance and surgical site infection rates have continued to be below national expected SSI rates.
Pain Management
Our orthopedic teams have been evaluating current postoperative pain management protocols to develop methods that will help decrease opioid administration.
Risk Stratification
Columbia’s joint reconstruction and spine specialists are leading efforts to apply formal risk stratification tools, including validated measures of severity scores, to better identify patients at highest risk for surgical complications that could affect their perioperative course. These risk stratification tools have provided important guidance to surgeons and the healthcare teams and are now used with every patient who presents for spine or joint surgery. The information acquired is then used to direct resources for patient optimization and also to advise patients on modifiable risk factors, such as smoking, cardiac issues, and diabetes management, that can be addressed preoperatively so that they can undergo surgery with a much lower risk profile.
A Dedicated Quality Infrastructure
When the Department of Orthopedic Surgery at NewYork-Presbyterian/Columbia established a program in quality and safety four years ago, William N. Levine, MD, Orthopedics Surgeon-in-Chief, and Dr. Michael Vitale created a formal infrastructure to drive a multidisciplinary effort for improving quality, safety, value, satisfaction, and the overall patient experience for all adult and pediatric orthopedic subspecialties.
This infrastructure has continued to expand, incorporating all the major aspects of a quality and safety program. Kevin Wang serves as the on-site quality officer for the Department, providing all physicians with information that supports quality improvement. These include risk stratification tools and risk severity scores to better identify patients at highest risk for surgical complications and surgeon-specific dashboards that detail performance for select quality, safety, value, and satisfaction metrics that are drilled down to the origin of the safety issue in order to define actionable data.
In addition, the data infrastructure facilitates valuable feedback. For example, not only are surgeons notified quickly if any of their patients have been readmitted, reviewing outcomes also provides important opportunities for changing practices that could lead to fewer readmissions. Over the past three years, readmissions for Columbia Orthopedics have steadily declined with rates lower than national and local benchmarks for all the major subspecialties.
In a survey of 35 orthopedic department chairs, it was found that the departments that have a dedicated infrastructure and faculty leadership for safety and quality efforts have lower risk-adjusted complication rates.
Columbia Orthopedics Quality Infrastructure and Leadership
Robert J. Strauch, MD & Mark Weidenbaum, MD
Compliance and Quality Assurance
Responsibilities: Quality Indicators, Documentation, Keep Safe Review, Root Cause Analysis
Charles M. Jobin, MD
Residency Program Director
Medical Education
Responsibilities: Morbidity and Mortality, Chief Quality Resident, Quality Improvement Curriculum, Quality Journal Club
Michael G. Vitale, MD, MPH
Vice Chief, Quality and Strategy
Transformational Quality Improvement
Responsibilities: Surgical Hip and Femur Fracture/ Comprehensive Care Joint Replacement Model, Spine SSI Protocol, Pay for Performance, Deep Vein Thrombosis, Lean Management, Tiered Huddles
H. John Cooper, MD
Public Facing Initiatives
Responsibilities: Regional Collaboratives, Quality Improvement CME (Spine Safety Summit), Newsletter Quality Columns, Faculty Practice Organization Quality Strategy
Kevin Wang, MHA
Director, Quality and Value
Data Infrastructure
Responsibilities: Dashboards, Value, National Benchmarking
Columbia Orthopedics has fewer 30 day inpatient readmissions than comparable benchmarks.
30 Day Readmission Rates — 2017
Foot and Ankle
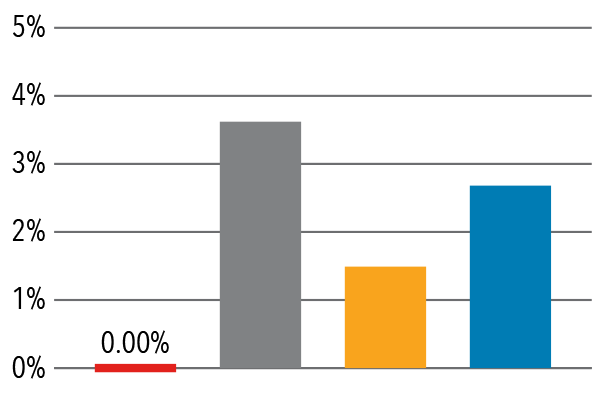
Hand/Microvascular
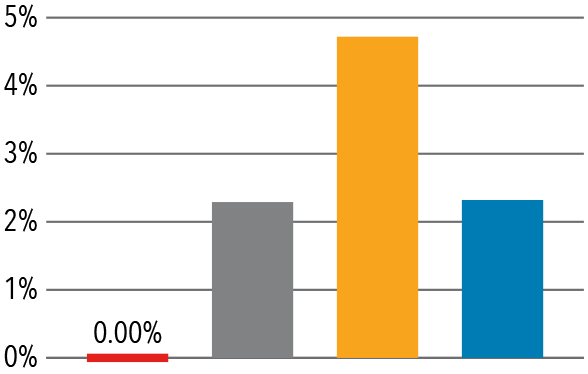
Pediatrics
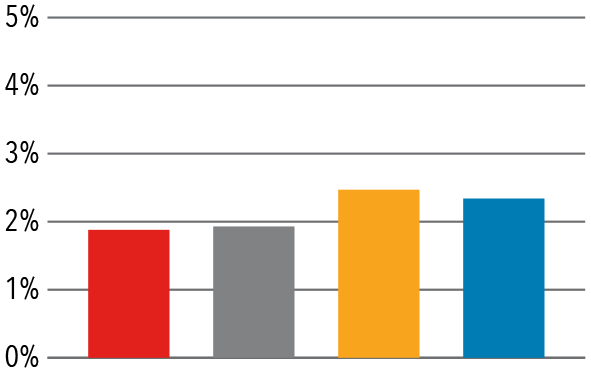
Shoulder/Elbow
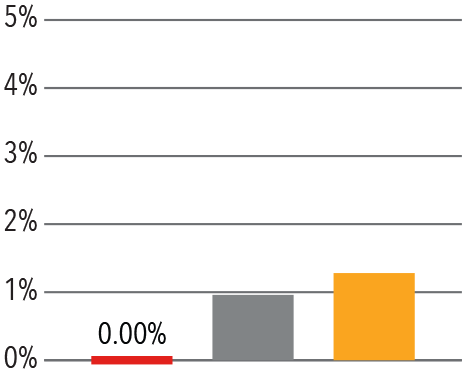
Adult Spine
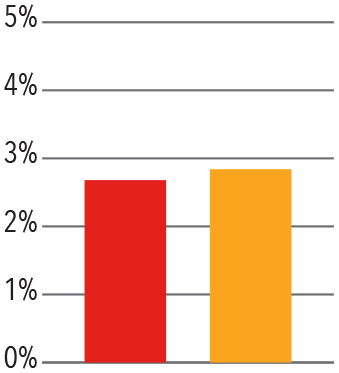
Pediatric Spine
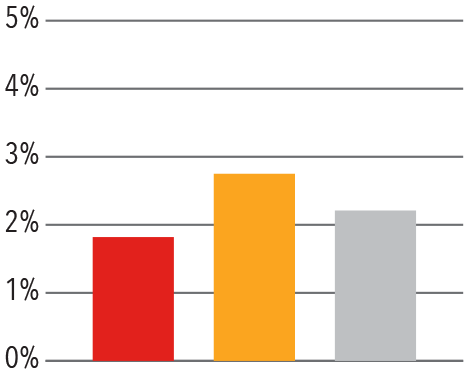
Trauma
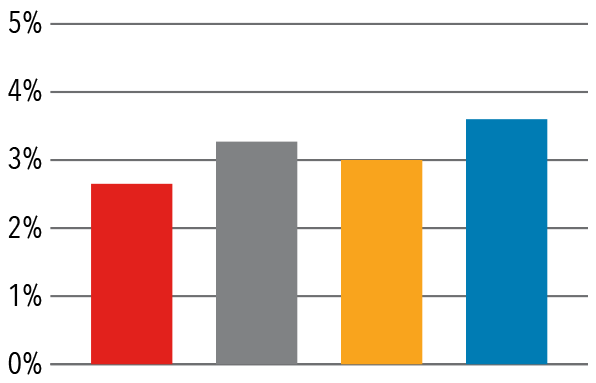
Source: Vizient/University Health Consortium, 2017
Safety and Spine Surgery Summit
On April 20, 2018, the Department of Orthopedic Surgery at NewYork- Presbyterian/Columbia hosted the 3rd Annual Safety in Spine Surgery Summit. Since its debut in 2016, the Summit has steadily grown in scope and attendance, with a standing-room-only crowd in 2018. “The appetite for information regarding safety in spine surgery is seemingly endless,” says Dr. Vitale, Chair of the Spine Surgery Summit. “This event is an impactful opportunity to learn from each other.”
The program featured a collaboration by spine surgeons in attendance on a best practice guideline for pediatric spine deformity. The consensus-based practice guidelines — the first-ever developed for preoperative halo gravity traction — included 42 items culled from a survey administered to nationwide experts in pediatric spine deformity asking ideal practices prior to the Summit meeting. The collaborators note that “the best practice guidelines provide new surgeons a place to begin their practice of halo gravity traction and drive future research.”
4th Annual Safety in Spine Surgery Summit
April 26, 2019 — New York City
The 4th Annual Safety in Spine Surgery Summit will feature sessions on:
-
Best practices for safety in spine surgery
-
Using tools to reduce variability and improve predictability of achieving positive outcomes
-
The importance of safety on the macroeconomic level
-
How to design talent, culture, and teams to achieve best outcomes
-
Protecting surgeons and providers
-
Value-based care in spine with all stakeholders
For more information, visit safetyinspinesurgery.com.